Osteoarthritis (OA) is a chronic joint disease characterized by degenerative changes in joint cartilage and secondary bone hyperplasia. It involves not only joint cartilage but also other intra-articular structures, including the subchondral bone, synovium, joint capsule, and others. The disease commonly affects weight-bearing joints such as the knee and hip. It is also referred to as osteoarthropathy or degenerative arthritis.
Etiology
The cause of primary osteoarthritis remains unclear. Its onset and progression are long-term, chronic, and gradual processes. It is generally believed to result from the combined effects of multiple pathogenic factors, including mechanical and biological factors. Age is a well-recognized risk factor, predominantly affecting middle-aged and elderly individuals. Other contributing factors include gender, obesity, genetics, inflammation, and metabolism, with a higher prevalence among females compared to males.
Secondary osteoarthritis can occur in young and middle-aged individuals, often as a result of trauma, infection, joint instability, or congenital conditions. It develops as a degenerative change in joint cartilage superimposed on pre-existing localized lesions.
Pathology
The primary pathological changes include degeneration, wear, and loss of joint cartilage; subchondral bone sclerosis or cystic changes; osteophyte formation at joint margins; synovial proliferation; thickening and contracture of joint capsules and surrounding ligaments; and atrophy of periarticular muscles. Ultimately, the articular surface may become completely destroyed, leading to joint deformities.
Joint Cartilage
In the early stages, cartilage becomes pale yellow and loses its luster, followed by localized softening and loss of elasticity. During weight-bearing activities, the cartilage undergoes wear, causing the surface to become rough, fragmented, and detached, forming loose bodies within the joint and exposing the subchondral bone.
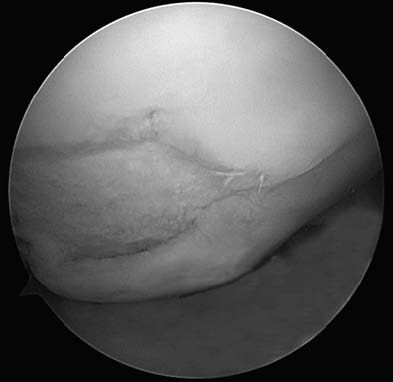
Figure 1 Arthroscopic pathological changes in cartilage in knee osteoarthritis
Subchondral Bone
In the central region where cartilage damage is most severe, subchondral bone density increases, and trabeculae become thickened, a condition termed "ivory-like changes." In peripheral regions with less stress, subchondral bone undergoes absorption, leading to cystic changes, often with sclerotic walls.
Osteophyte Formation
At the edges of cartilage or sites of tendon attachment, osteophyte formation occurs due to vascular proliferation and active chondrocyte metabolism, resulting from endochondral ossification.
Synovium
Early pathological changes include proliferative synovitis, characterized by congestion, edema, and increased synovial fluid secretion. In later stages, fibrous synovitis develops, with reduced synovial fluid and replacement of proliferative synovium by fibrous tissue strands.
Joint Capsule, Ligaments, and Muscles
Fibrosis and thickening of joint capsules and ligaments occur, limiting joint mobility. Pain causes protective muscular spasms around the joint, further restricting activity; in later stages, muscle atrophy develops.
Clinical Manifestations
Pain is the primary symptom, with joint mobility limitation and deformities being common accompanying features.
Joint Pain and Tenderness
In the early stages, pain is mild or moderate, intermittent, and dull, often alleviated by rest and aggravated by activity. Pain is frequently influenced by weather conditions. In later stages, persistent pain or nighttime pain may occur. Local tenderness is often prominent, particularly during joint swelling.
Joint Stiffness
Morning stiffness after waking, referred to as "morning stiffness," is often present and improves with activity. Stiffness becomes more pronounced under conditions of low atmospheric pressure or high humidity. Stiffness generally lasts for a short duration, typically less than 30 minutes.
Movement Disorders
Pain, muscle atrophy, soft tissue contracture, or intra-articular loose bodies may cause joint instability, locking, or inability to fully flex and extend.
Joint Deformity
Obvious joint enlargement and deformity may occur in hand osteoarthritis, with the appearance of Heberden’s nodes and Bouchard’s nodes. In the knee joint, effusion and osteophyte formation can cause swelling and, in some cases, varus or valgus deformities.
Crepitus
Due to cartilage destruction and roughening of joint surfaces, crepitus is often heard or felt during joint movement, commonly in the knee joint.
Auxiliary Examinations
Laboratory Tests
Indicators such as routine blood tests, protein electrophoresis, immune complexes, and serum complement levels are generally within normal ranges. During phases of synovial inflammation, mild elevations in C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) may be observed.
Imaging
X-ray examination is the most commonly used diagnostic tool. Typical findings include asymmetric narrowing of the joint space, subchondral bone sclerosis or cystic changes, osteophyte formation at joint margins, and intra-articular loose bodies in some cases. In severe cases, deformities such as knee varus can be seen.

Figure 2 X-ray findings in knee osteoarthritis
Diagnosis and Differential Diagnosis
Diagnosing osteoarthritis is generally straightforward based on the patient’s symptoms, clinical signs, and characteristic findings on X-ray imaging.
The main differential diagnoses include:
Rheumatoid Arthritis
This primarily affects young and middle-aged women, characterized by symmetrical involvement of multiple joints, often affecting the small joints of both hands, especially the proximal interphalangeal joints. Large joints such as the hip and knee may also be involved. Morning stiffness lasting more than one hour is typical. Affected joints exhibit swelling, pain, and restricted movement during episodes, with residual functional impairment or joint deformity after the symptoms subside. Extra-articular manifestations are common, including anemia, weight loss, and systemic symptoms, particularly during early stages. Subcutaneous rheumatoid nodules are present in 20–30% of cases. Laboratory tests often reveal elevated erythrocyte sedimentation rate (ESR), increased C-reactive protein (CRP), and positive rheumatoid factor.
Gouty Arthritis
This predominantly affects men, presenting as asymmetric, acute-onset joint redness, swelling, pain, and elevated skin temperature. It most commonly involves the first metatarsophalangeal joint, ankle, and knee. Episodes are often associated with high-purine diets. Laboratory findings may show elevated serum uric acid levels, although normal uric acid levels can sometimes be observed during acute flare-ups.
Ankylosing Spondylitis
This commonly affects young men, initially presenting with pain in the bilateral sacroiliac joints and lower back. The condition progresses to involve the thoracic and cervical spine, leading to spinal ankylosis. Hip and knee joints may also be affected, typically in a symmetrical manner. Laboratory tests reveal elevated ESR, and HLA-B27 positivity is highly specific. X-rays often show sacroiliitis and a bamboo spine appearance.
Pigmented Villonodular Synovitis (PVNS)
This typically occurs between the ages of 20 and 30, with a nearly equal prevalence in men and women. Usually presents as unilateral knee involvement with joint swelling and pain. Palpable proliferative synovial tissue with a firm texture is often detectable. MRI findings include thickened synovium and villous proliferations, with low signal intensity on both T1- and T2-weighted sequences due to iron deposition. Joint aspiration commonly reveals dark or coffee-colored hemorrhagic fluid.
Treatment
The primary goals of treatment are to alleviate pain, improve joint function, slow disease progression, and correct deformities.
Basic Treatments
Patient Education
Weight reduction and load minimization are recommended, along with modifications to physical activities. Activities such as prolonged running, jumping, squatting, climbing stairs or hills are minimized, while aerobic exercises such as swimming and cycling are preferred. Flexion-extension movements and muscle-strengthening exercises under non-weight-bearing conditions can improve joint function.
Physical Therapy
Techniques such as thermotherapy, hydrotherapy, ultrasound therapy, acupuncture, massage, and transcutaneous electrical nerve stimulation (TENS) are used to enhance local circulation and reduce inflammation.
Mobility Support
Devices such as canes, crutches, or walkers can be used to reduce joint loading.
Orthotic Support
Appropriate orthotic devices or corrective footwear are employed to address varus or valgus deformities, redistribute load lines, and balance the load across joint surfaces.
Pharmacological Treatments
Topical Analgesics
Topical formulations of nonsteroidal anti-inflammatory drugs (NSAIDs) such as gels, creams, patches, and ointments are effective for mild to moderate joint pain with minimal side effects.
Systemic Analgesics
These include oral, injectable, or suppository forms of NSAIDs. Caution is advised due to potential side effects affecting the gastrointestinal tract, cardiovascular system, and kidneys.
Intra-Articular Injections
Hyaluronic Acid
Injection of sodium hyaluronate provides lubrication, protects joint cartilage, and alleviates pain.
Corticosteroids
Intra-articular corticosteroid injections offer rapid pain relief but may accelerate cartilage degeneration and disease progression. Repeated or indiscriminate corticosteroid injections into the joint cavity are not advised.
Surgical Treatments
The main objectives of surgery include:
- Relieving pain
- Correcting deformities
- Improving joint function
Depending on the severity of the condition, the following surgical options are available:
- Arthroscopic Debridement: Effective in removing loose bodies, damaged meniscus fragments, and intra-articular debris.
- Joint Realignment Surgery: For knee osteoarthritis, this involves procedures such as high tibial osteotomy or, more recently, proximal fibular osteotomy, which has shown promising efficacy.
- Joint Replacement Surgery: Suitable for patients with severe osteoarthritis, knee replacement options include unicompartmental arthroplasty, patellofemoral joint replacement, and total knee arthroplasty. For hip joint osteoarthritis, total hip arthroplasty is the preferred option.
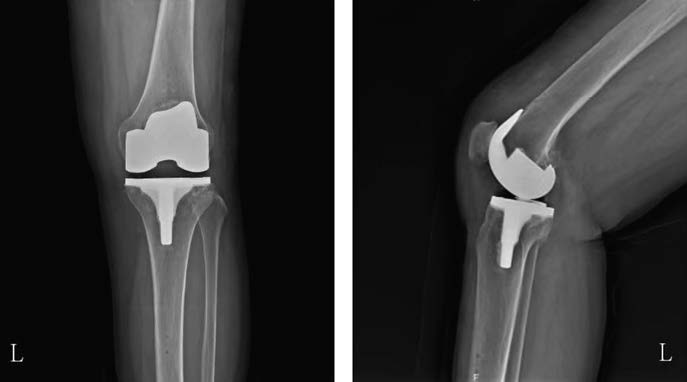
Figure 3 X-ray findings post total knee arthroplasty in knee osteoarthritis

Figure 4 X-ray findings before and after total hip arthroplasty for hip osteoarthritis