Knee joint tuberculosis is the second most common type of osteoarticular tuberculosis, following spinal tuberculosis. It is frequently observed in children and adolescents, primarily involving the distal femur and proximal tibia. Synovial tuberculosis is more common than osseous tuberculosis.
Pathology
The synovium of the knee joint is highly vascularized, making synovial tuberculosis the most common initial presentation. It is characterized by inflammatory infiltration and effusion, leading to joint swelling and effusion. The lesion gradually invades the bone at the attachment sites of the synovium, resulting in marginal bone erosion. The process progresses subchondrally, causing large areas of cartilage to detach and leading to total joint tuberculosis. In advanced stages, the accumulation of pus forms cold abscesses, which may rupture to form chronic sinus tracts. Destruction of ligamentous structures often results in pathological subluxation or dislocation. Once the lesion stabilizes, fibrous ankylosis of the knee joint may develop, sometimes accompanied by flexion contracture.
Clinical Presentation
The condition typically has an insidious onset and is accompanied by systemic symptoms such as low-grade fever, fatigue, listlessness, poor appetite, weight loss, and anemia. Elevated erythrocyte sedimentation rate (ESR) is often observed. In children, nocturnal crying is commonly reported. The superficial location of the knee joint makes swelling and effusion particularly evident. On examination, findings often include fullness of the popliteal fossa, enlargement of the suprapatellar bursa, and a positive patellar ballottement test. In more advanced cases, there may be significant synovial swelling and thickening.
Early joint aspiration may yield clear fluid, but as the disease progresses, the aspirated fluid tends to become increasingly turbid, containing fibrinous material, eventually becoming purulent. Persistent joint effusion and disuse muscle atrophy result in spindle-shaped swelling of the knee. Pain leads to a flexed position of the joint, which, over time, causes flexion contracture. In advanced stages, cold abscesses form, and rupture leads to chronic sinus tracts that fail to heal. Ligament destruction may result in pathological dislocation. Once the lesion stabilizes or heals, fibrous ankylosis occurs. Bone growth suppression often leads to limb length discrepancies.
Imaging and Arthroscopy
In the early synovial tuberculosis stage, X-rays typically show only suprapatellar bursal swelling and localized osteoporosis. In long-standing cases, progressive narrowing of the joint space and marginal bone erosion are evident. Advanced stages are characterized by severe bone destruction, complete loss of the joint space, and posterior subluxation of the tibia. Severe osteoporosis is observed unless mixed infections are present, in which case bone sclerosis is noted.
CT and MRI imaging provide a more detailed visualization of lesions that cannot be detected on conventional X-rays. MRI, in particular, is valuable for early diagnosis.
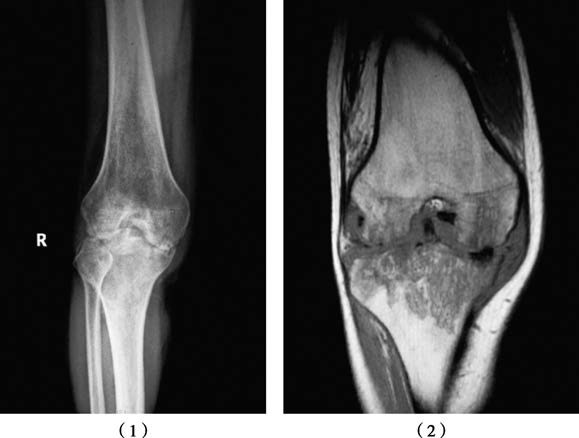
Figure 1 Plain X-ray of knee joint tuberculosis (1) and MRI (2)
Arthroscopy has a unique role in the early diagnosis of knee synovial tuberculosis. It allows for joint fluid culture, tissue biopsy, and synovectomy to be performed under direct observation.
Treatment
Systemic Treatment
Due to its superficial location, knee joint tuberculosis can often be identified early. For isolated synovial tuberculosis, about 80% of cases achieve resolution with systemic anti-tuberculosis drug therapy, preserving normal or near-normal joint function. Anti-tuberculosis drugs are administered during active disease and in the pre- and post-operative periods.
Non-Surgical Treatment
Joint Aspiration and Drug Injection
Effusion is aspirated, followed by intra-articular injection of anti-tuberculosis drugs. Adults may receive 200 mg of isoniazid per injection, while the dosage is halved for children. Injections are administered 1–2 times per week, with a course lasting 3 months. Synovectomy is generally not recommended in early cases because anti-tuberculosis drugs are sufficient to control the disease.
Immobilization
Activity limitation, rest, and lower limb traction or plaster immobilization are utilized to stabilize the joint.
Sinus Tract Treatment
Drainage and medication are used in cases of mixed infections with sinus tract formation.
Surgical Treatment
Synovectomy
If there is no improvement after local drug therapy and synovial swelling persists with thickening, synovectomy may be considered. Arthroscopic synovectomy offers advantages such as minimal invasiveness, fewer complications, faster recovery, better efficacy, and lower cost.
Debridement Surgery
In cases of total joint tuberculosis with significant progression or abscess formation, lesion debridement is needed. Patients under 15 years of age are generally only treated with debridement. In those over 15 years old with severe joint destruction and deformity, debridement can be followed by knee arthrodesis. Patients with sinus tracts or flexion contractures are also candidates for joint arthrodesis.
Total Knee Replacement
If the tuberculosis lesion has been fully controlled and the disease remains inactive for over 10 years, total knee replacement may be considered. However, the risk of reactivating latent tuberculosis lesions post-surgery requires careful consideration.