Characteristics of Onset
Bone and joint tuberculosis is a secondary infectious disease caused by the invasion of Mycobacterium tuberculosis into bones or joints. Tuberculosis is one of the leading causes of death from infectious diseases among adults worldwide. Bone and joint tuberculosis is the most prevalent form of extrapulmonary secondary tuberculosis, with the vast majority of primary lesions originating from pulmonary tuberculosis, accounting for approximately 5%–10% of tuberculosis cases. Among them, spinal tuberculosis is the most common, constituting over 50% of cases, while hip and knee tuberculosis each account for approximately 15%. The common sites of bone and joint tuberculosis are typically weight-bearing, highly mobile, and injury-prone regions. High-risk populations include individuals with a history of tuberculosis infection, immigrants from high-prevalence areas, people with diabetes or chronic kidney disease, malnourished individuals, long-term users of immunosuppressants, and AIDS patients. Patients often have a personal or family history of tuberculosis. The condition may occur at any age, and there is no significant difference in incidence between genders.
Pathology
The primary pathogen is Mycobacterium tuberculosis of the human type. The bacteria typically do not directly invade bones or the synovial membranes of joints to cause bone and joint tuberculosis but rather spread secondarily from primary lesions in the lungs or gastrointestinal tract via hematogenous dissemination. The initial pathological change in bone and joint tuberculosis is either simple synovial tuberculosis or simple osseous tuberculosis, with the latter being more common. In the early stages, the lesion remains localized to the metaphysis of long bones, and the articular cartilage remains intact. If tuberculosis is effectively controlled at this stage, joint function remains unaffected. However, if the lesion progresses further, it may spread to the joint cavity and destroy the articular cartilage, leading to what is known as total joint tuberculosis. Uncontrolled total joint tuberculosis may rupture, forming sinus tracts that discharge caseous necrotic material and pus, resulting in secondary infection. At this stage, joint destruction is complete, leaving various degrees of joint dysfunction.
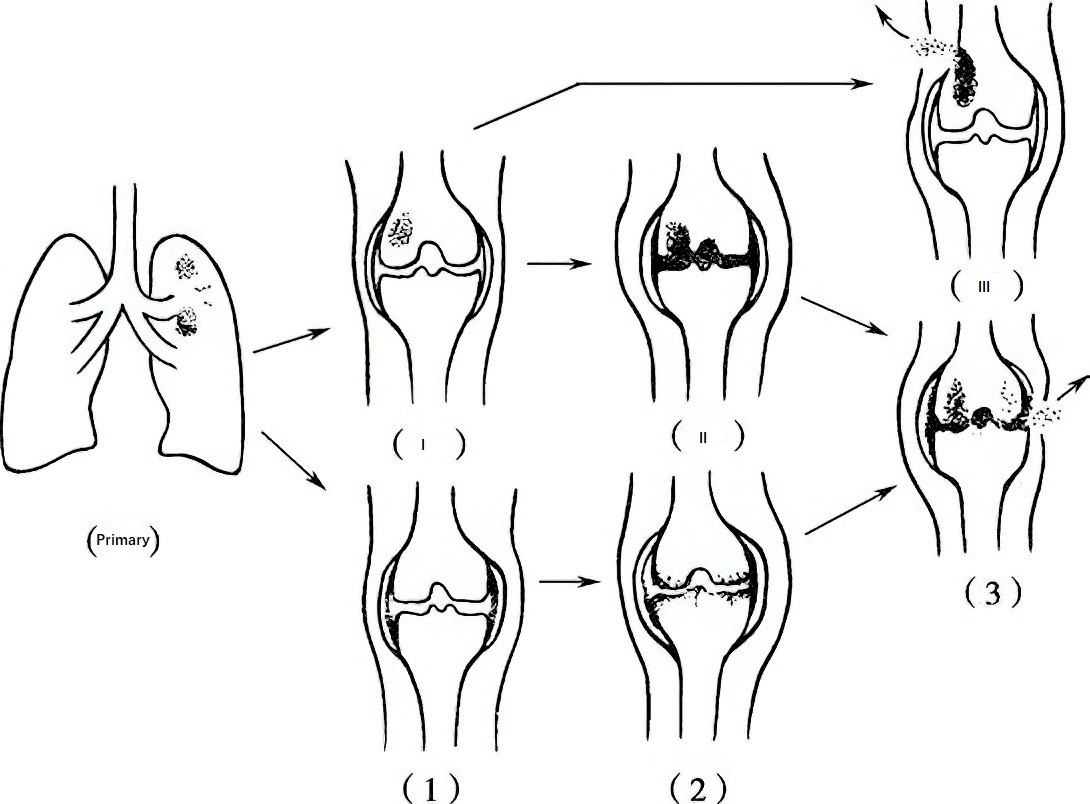
Figure 1 Schematic diagram of the clinico-pathological progression of bone and joint tuberculosis
(Primary) Primary focus
(I) Simple osseous tuberculosis
(II) Advanced joint tuberculosis arising from osseous tuberculosis
(III) Simple osseous tuberculosis rupturing through skin, forming sinus tract
(1) Simple synovial tuberculosis
(2) Advanced joint tuberculosis arising from synovial tuberculosis
(3) Advanced joint tuberculosis rupturing through skin, forming sinus tract
Clinical Manifestations
Systemic Symptoms
The onset is often gradual, with insidious symptoms. There may be no obvious systemic tuberculosis intoxication symptoms or only mild ones, including low-grade fever in the afternoon, fatigue, and diaphoresis. Typical cases may also present with weight loss, poor appetite, and anemia. In rare cases of acute onset, particularly in children, high fever may occur.
Clinical Manifestations of Spinal Tuberculosis
Details are provided in the section "Spinal Tuberculosis."
Clinical Manifestations of Joint Tuberculosis
Details are provided in the sections "Hip Joint Tuberculosis" and "Knee Joint Tuberculosis."
Tuberculous Abscess
As the condition progresses, the affected area may accumulate pus, tuberculous granulation tissue, sequestra, and caseous necrotic tissue. Unlike acute inflammatory abscesses, tuberculous abscesses do not exhibit signs of redness, heat, or other acute inflammatory responses and are therefore referred to as "cold abscesses." The abscess may spread along tissue planes, forming abscesses at distant sites from the original lesion. When the abscess ruptures through the skin, it creates a sinus tract, discharging rice-water-like pus, often mixed with necrotic materials or sequestra, which is referred to as an external fistula. The abscess may also communicate with internal visceral organs, forming internal fistulas. For example, the abscess may drain into the esophagus, lungs, intestines, or bladder, resulting in the discharge of pus through coughing, feces, or urine. When cold abscesses rupture and mixed infections occur, acute inflammatory reactions may develop locally. If these secondary infections are not controlled, they may result in chronic wasting, anemia, systemic toxicity, and, in severe cases, liver or kidney failure, or even death.
Sequelae
Following the resolution of late-stage lesions, various sequelae may develop, including:
- Joint dysfunction, such as joint ankylosis.
- Deformities, such as flexion contracture deformities of joints or kyphotic deformities of the spine.
- Limb length discrepancies, such as unequal lengths of the lower limbs.
Laboratory Examinations
Hematology
Routine blood tests may show mild anemia. The white blood cell count is generally normal, with only about 10% of patients showing an elevated white blood cell count. Erythrocyte sedimentation rate (ESR) is significantly increased during the active phase of the disease but is usually normal during the quiescent phase, serving as an important indicator for assessing whether the lesion is inactive or has relapsed. C-reactive protein (CRP) levels are closely related to the severity of the inflammatory response, making CRP a useful marker for diagnosing the activity of tuberculosis and evaluating clinical efficacy.
Bacteriology
Acid-Fast Staining for Microscopy
Acid-fast staining allows for rapid detection of acid-fast bacilli in aspirated pus samples from bone or joint tuberculosis. It is a classic diagnostic method for bone and joint tuberculosis. Its advantages include simplicity, rapid results, and low cost. However, it has low sensitivity and poor specificity.
Mycobacterium tuberculosis Culture
A positive culture is an important diagnostic criterion for bone and joint tuberculosis. However, due to the slow growth of Mycobacterium tuberculosis, it typically takes 4–8 weeks to obtain results, and the positive rate is only 30%–50%. As it is time-consuming and has a low positive rate, its clinical application has become less frequent.
Immunology
Diagnostic methods based on antigens or antibodies derived from Mycobacterium tuberculosis are used to detect tuberculosis antibodies or antigens in the patient's serum. These methods are characterized by rapid results, simplicity, and relatively high sensitivity and specificity.
Tuberculin Test
The purified protein derivative (PPD) skin test for tuberculosis is based on the principle of type IV hypersensitivity. It has low sensitivity and specificity, meaning that test results cannot be directly used to confirm or rule out tuberculosis. A strongly positive result may support a diagnosis of tuberculosis in adults or indicate recent tuberculosis infection, although not yet active disease. In children, especially those under one year of age, it may serve as a diagnostic criterion for tuberculosis.
T-Cell Spot Test (T-SPOT.TB)
This newer diagnostic approach for bone and joint tuberculosis has been developed based on enzyme-linked immunospot (ELISPOT) assays. It uses peripheral blood samples to detect specific effector T-cells from tuberculosis-infected individuals. It has relatively high sensitivity and specificity but also carries a certain false-positive rate.
Serum Tuberculosis Antibodies
Tuberculosis antibodies are present in various body fluid specimens. Serum tuberculosis antibody detection is reproducible, simple, fast, cost-effective, and has high sensitivity and specificity. It is widely used as an auxiliary diagnostic method for tuberculosis.
Molecular Biology
DNA detection techniques for Mycobacterium tuberculosis allow for direct classification of strain lineages and antimicrobial susceptibility testing. These methods are characterized by ease of operation, rapid reactions, high sensitivity, and high specificity.
Fluorescent Quantitative PCR (FQ-PCR)
This is a modern nucleic acid quantification technique that has advanced from qualitative to quantitative detection compared to conventional PCR. It is more specific, reproducible, and allows for a higher degree of automation.
Xpert MTB/RIF
This is an advanced, fully automated molecular diagnostic method for tuberculosis and rifampicin-resistant tuberculosis. It provides rapid, accurate, and easy-to-operate results. It is currently recommended by the World Health Organization (WHO) for the diagnosis of extrapulmonary tuberculosis and rifampicin resistance.
Loop-Mediated Isothermal Amplification (LAMP)
This is a unique nucleic acid (DNA) amplification method. It is simple to perform, highly specific, and an effective rapid diagnostic tool for tuberculosis. It is also recommended by WHO for tuberculosis diagnosis.
Pathology Examination
Percutaneous biopsy of the lesion or pathological and microbiological examinations following surgery are critical for confirming the diagnosis. Pathological examination showing typical tuberculous granulomas, combined with microbiological evidence (e.g., from smear microscopy or other bacteriology assays) proving infection by Mycobacterium tuberculosis, is the basis for a definitive diagnosis. During procedures such as debridement of tuberculosis lesions, it is essential to collect bacterial specimens for laboratory testing. Combining bacteriology and pathology examinations improves diagnostic accuracy.
Imaging Examinations
X-Ray Examination
X-ray imaging plays a key role in the diagnosis of bone and joint tuberculosis, but abnormalities typically appear only 6–8 weeks after disease onset, limiting early diagnosis. Characteristic findings include localized osteopenia, destruction of bone with minimal surrounding calcification, and soft tissue swelling. Over time, cystic changes with clear boundaries, pronounced sclerosis, and periosteal reactions may occur. Findings such as sequestration and pathological fractures may also appear.
CT (Computed Tomography)
CT provides two-dimensional or three-dimensional images and offers more detailed information compared to plain X-rays. It can clearly delineate the location of lesions, sequestra, and the extent of soft tissue involvement. It is particularly useful for visualizing surrounding cold abscesses. CT guidance can also assist with aspiration and biopsy procedures.
MRI (Magnetic Resonance Imaging)
MRI can display abnormal signals during the early inflammatory infiltration phase of tuberculosis, making it more sensitive than other imaging methods for early diagnosis. It provides better visualization of the extent of lesions, soft tissue abnormalities, bone destruction, intervertebral disc involvement, and compression of the spinal cord and nerves within the spinal canal. MRI is valuable in distinguishing tuberculosis from spinal tumors, infections, fractures, and degenerative diseases.
Ultrasound
Ultrasound is useful for identifying the size and location of deep cold abscesses. It can also guide percutaneous aspiration for smear and bacterial culture.
Arthroscopy
Arthroscopy, combined with synovial biopsy, proves valuable for diagnosing synovial tuberculosis.
Treatment
Management of bone and joint tuberculosis requires a comprehensive approach, including rest, convalescence, proper nutrition, standardized chemotherapy, and surgical treatment if needed. Of these, anti-tuberculosis drug therapy plays a central role and extends throughout the entire treatment process.
Systemic Treatment
Supportive Therapy
Efforts should be made to ensure adequate rest and avoid overexertion. Nutritional intake should be optimized with sufficient daily protein and vitamin supply. For patients with anemia, correcting anemia is necessary.
Anti-Tuberculosis Drug Therapy
The principles of anti-tuberculosis medication for bone and joint tuberculosis are:
- Early initiation,
- Combination therapy,
- Appropriate dosage,
- Consistent use, and
- Full treatment adherence. Strict adherence to prescribed regimens ensures therapeutic efficacy and helps to control and resolve lesions.
Commonly used first-line anti-tuberculosis drugs include isoniazid (INH), rifampin (RFP), pyrazinamide (PZA), streptomycin (SM), and ethambutol (EMB). Current treatment regimens involve a two-phase approach: an intensive phase with a four-drug combination (isoniazid, rifampin, pyrazinamide, and ethambutol) followed by a continuation phase with a three-drug combination (isoniazid, rifampin, and ethambutol). Isoniazid and rifampin are preferred as the first-line drugs. Due to its neurotoxicity affecting the eighth cranial nerve, streptomycin is no longer considered a preferred agent.
The duration of treatment for extrapulmonary tuberculosis is generally 12 months. For bone and joint tuberculosis, expert consensus suggests the following treatment durations:
- For children, no less than 12 months.
- For adults, 12–18 months, extendable to 18–24 months if necessary.
Main adverse reactions to anti-tuberculosis drugs include hepatotoxicity, neurotoxicity, allergic reactions, gastrointestinal disturbances, and renal toxicity. Regular liver and kidney function tests are necessary during the course of treatment, and hepatoprotective medication is often prescribed concurrently. In case of adverse reactions, timely adjustments are required. Ethambutol use in children requires caution. Recent studies have demonstrated significant inhibitory effects of quinolone antibiotics on Mycobacterium tuberculosis.
After anti-tuberculosis drug therapy, systemic and localized symptoms gradually diminish. The effectiveness of treatment should be assessed comprehensively, considering the patient's symptoms, clinical examination findings, laboratory test results, imaging studies, and long-term follow-ups. The criteria for determining treatment cure include:
- Stable general condition, normal body temperature, and good appetite,
- Disappearance of local symptoms, pain relief, and closure of sinus tracts,
- Normalization of ESR in three consecutive tests,
- Reduction or complete resolution of abscesses on imaging, calcification of lesions, absence of sequestra, and clear lesion margins, and
- Maintenance of these criteria for one year after resuming ambulation.
Once these criteria have been met, anti-tuberculosis drug therapy can be discontinued; however, regular follow-ups are still required.
Drug-resistant tuberculosis treatment regimens are typically formulated based on drug susceptibility test results and the patient's prior treatment history. According to the 2020 WHO guidelines for drug-resistant tuberculosis, treatment regimens of 18 months or longer are recommended.
Local Treatment
Local Immobilization
Methods include plaster casts, braces, or traction. The aim is to allow the affected area to rest, relieve pain, and stabilize the lesion. Clinical practice has shown that combining systemic drug therapy with local immobilization achieves better outcomes.
Local Drug Injections
Local injection therapy with anti-tuberculosis drugs enables high local drug concentration with minimal systemic reactions. It is most suitable for early cases of simple synovial tuberculosis. Commonly used drugs include isoniazid at a dosage of 100–200 mg, given 1–2 times per week depending on the amount of joint effusion. Reducing joint effusion and the appearance of clearer fluid after repeated aspiration signify therapeutic effectiveness, and injections can be continued. Ineffectiveness may necessitate a change in treatment. Repeated aspiration and drug injections into cold abscesses are generally discouraged due to the risk of mixed bacterial infections and sinus tract formation.
Surgical Treatment
Incision and Drainage of Abscesses
For cold abscesses with mixed infections, high fever, or severe systemic symptoms, incision and drainage can be performed if the patient's condition precludes lesion debridement. After systemic improvement, lesion debridement may follow. However, incision and drainage often result in chronic sinus formation, complicating later procedures.
Lesion Debridement
Lesion debridement under systemic anti-tuberculosis drug therapy offers good outcomes and shortens treatment duration. Indications for surgery include:
- Lack of symptom relief despite standardized drug therapy,
- Presence of sequestra and large abscesses,
- Persistent sinus discharge, and
- Spinal instability, spinal cord or cauda equina compression, or severe kyphotic deformity in spinal tuberculosis.
Contraindications for surgery include:
- Active tuberculosis in other organs,
- Severe underlying systemic conditions, or
- Other comorbidities precluding surgery.
To reduce the risk of hematogenous spread of Mycobacterium tuberculosis during surgery, standardized preoperative anti-tuberculosis drug therapy for 2–4 weeks is required. Postoperatively, the full chemotherapy regimen must be completed.
Other surgical interventions include:
- Arthrodesis for cases of joint fibrous ankylosis, contracture, or instability,
- Osteotomy to correct joint or spinal deformities,
- Total joint replacement for patients with joint function loss, which can improve function if indications are strictly observed,
- Spinal decompression for symptoms of spinal cord or cauda equina compression, including paraplegia,
- Bone graft fusion with internal fixation for severe bone destruction and spinal instability.