Acute suppurative osteomyelitis occurs most commonly in children and adolescents and is characterized by bone destruction and resorption. It is frequently observed in the proximal tibia and distal femur, but it may also involve the distal tibia, proximal humerus, iliac bone, and other sites.
Etiology
The most common causative pathogen is Staphylococcus aureus, accounting for approximately 75% of cases, followed by Streptococcus pyogenes (group B streptococcus) and Gram-negative bacilli. Pathogenic bacteria typically originate from infection foci at other parts of the body, often in the skin or mucous membranes, such as boils, carbuncles, tonsillitis, or otitis media.
When the primary focus of infection is not properly managed, or in cases of reduced systemic resistance, malnutrition, or fatigue, bacteria may enter the bloodstream, resulting in bacteremia or even sepsis. Septic emboli can reach the nutrient arteries of bones and become lodged in the capillaries at the metaphysis of long bones due to the slow blood flow in this region. In children, the terminal arterioles and capillaries near the growth plate tend to form vascular loops, which are tortuous, rich in blood supply, and characterized by slow blood flow, making bacterial deposition more likely. As a result, the metaphysis of long bones is the most common site of involvement. Local trauma with subsequent tissue injury and bleeding may act as a triggering factor.
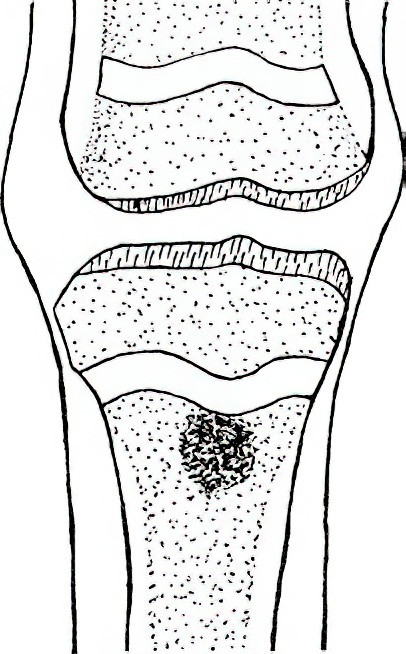
Figure 1 Schematic diagram of acute pyogenic osteomyelitis predilection site: Metaphysis of long bones in children
Pathology
The primary pathological changes include abscess formation, bone destruction, and periosteal new bone formation. Numerous septic emboli obstruct the small blood vessels at the metaphysis of long bones, leading to rapid bone destruction, along with congestion, exudation, and infiltration of white blood cells. Proteolytic enzymes released by white blood cells degrade both bacteria and necrotic bone tissue, forming an abscess that progressively enlarges, increasing intraosseous pressure. The abscess may continue to grow and merge with adjacent abscesses, spreading in various directions:
Spread to the Medullary Cavity
In children, the growth plate serves as a robust barrier to infection, preventing the spread of pus and bacteria through it. As a result, the abscess usually extends into the medullary cavity instead.
Extension through the Cortical Bone at the Metaphysis
Pus may spread along the Haversian canals to the subperiosteal layer, forming a subperiosteal abscess. It may eventually rupture through the periosteum, soft tissue, and skin, draining externally and forming a sinus tract. Bone immersed in the pus loses its blood supply and becomes dead bone (sequestrum). During the formation of sequestrum, adjacent periosteum responds to the inflammatory congestion and stimulation by the pus, producing new bone that encases the diaphysis or sequestrum, forming an "involucrum." The involucrum often contains small openings that communicate with sinus tracts on the skin. Within the involucrum, sequestrum, pus, and inflammatory granulation tissue are typically present. Poor drainage from this cavity leads to the formation of a chronic bone abscess. Small pieces of sequestrum may be absorbed by granulation tissue or cleared by phagocytes, or they may drain through sinus tracts. Larger pieces of sequestrum are more difficult to absorb or expel, often persisting in the body for long periods. The occurrence of sequestrum, bone cavities, sinus tracts, and involucrum marks the transition to the chronic stage of the disease.
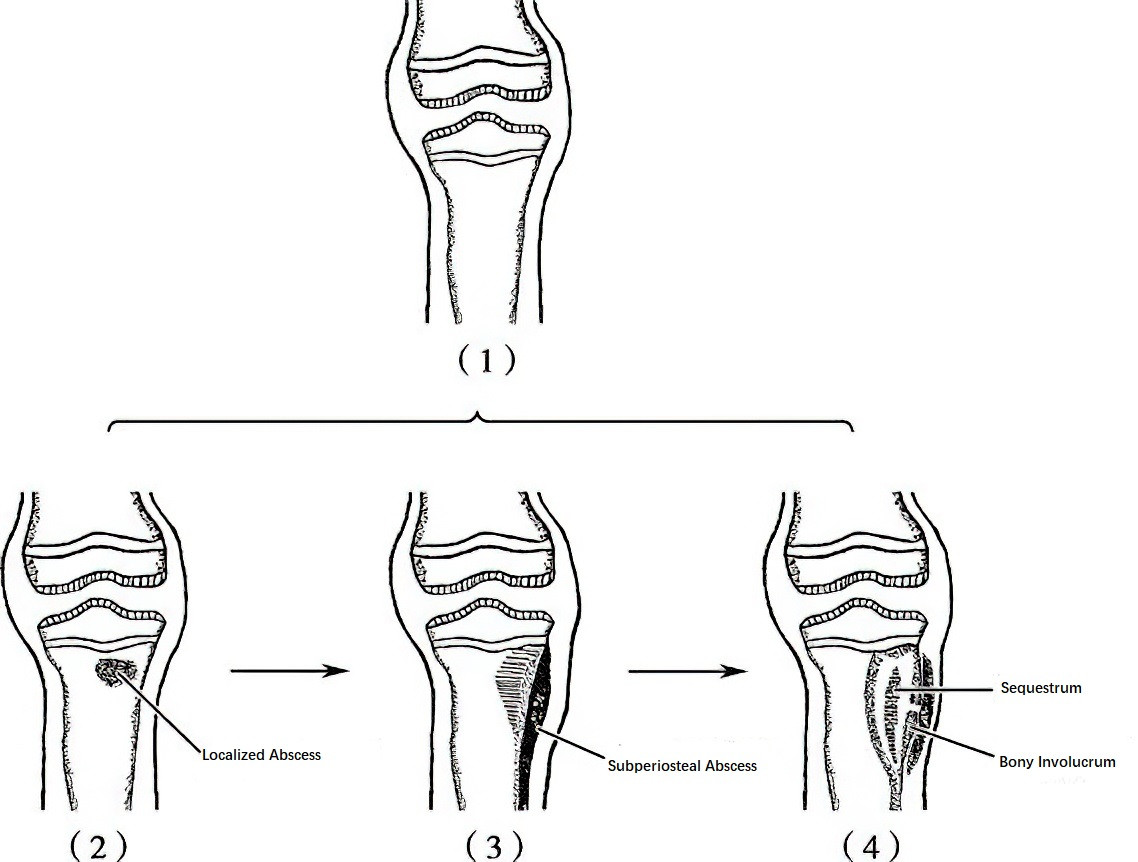
Figure 2 Pathological process of acute pyogenic osteomyelitis
(1) Normal (2) Localized Abscess (3) Pus Penetrates Under the Periosteum, Forming a Subperiosteal Abscess (4) Subperiosteal Abscess Gradually Enlarges, Ruptures Through the Periosteum into Soft Tissue, with Formation of Sequestrum and Involucrum
Spread to Joints
Due to the growth plate acting as a barrier in children, direct extension leading to septic arthritis is uncommon. However, in cases involving the metaphysis of the femur, which lies within the hip joint capsule, pus may rupture through the cortical bone and enter the joint cavity, resulting in septic arthritis of the hip.
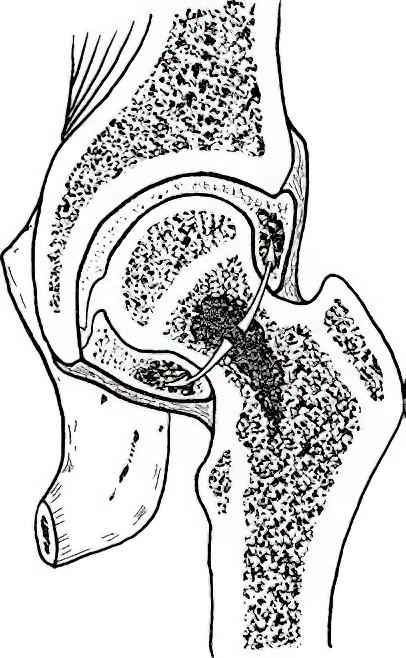
Figure 3 Schematic diagram of pus entering the joint cavity leading to pyogenic arthritis
Clinical Manifestations
Typical systemic symptoms include chills, high fever, nausea, and lethargy. The onset of illness is acute, often beginning with chills, followed by a high fever exceeding 39°C. Children may present with irritability, vomiting, or seizures, and severe cases may progress to coma or shock. The primary source of infection is often difficult to identify, although a history of trauma is common prior to symptom onset in children.
Severe pain develops early in the affected limb, accompanied by surrounding muscle spasms. Both active and passive movements may be resisted due to pain. Local skin temperature increases, but swelling is initially mild. The joint is often held in a semi-flexed position, and deep tenderness is present at the affected site. After several days, swelling intensifies, and tenderness worsens, indicating the formation of a subperiosteal abscess. When the abscess ruptures through the periosteum into the surrounding soft tissue, pain may decrease, while local redness, swelling, and warmth become more pronounced, with pronounced tenderness on light palpation. Reactive joint effusion may occur if the lesion is near a joint. As the abscess spreads along the medullary cavity, the area of swelling and pain increases. If the lesion involves the entire diaphysis, extensive bone destruction may lead to pathological fractures.
The natural progression of the disease typically lasts 3–4 weeks. Once the abscess ruptures through the periosteum, pain subsides rapidly, body temperature gradually decreases, and sinus tracts form, marking the transition to the chronic stage.
Auxiliary Examinations
Laboratory Tests
Laboratory findings include:
- Increased white blood cell count, with neutrophils exceeding 90%.
- Accelerated erythrocyte sedimentation rate (ESR).
- Elevated C-reactive protein (CRP), which is more sensitive than ESR.
Blood cultures can identify the causative pathogens, though cultures may sometimes fail, especially in cases where antibiotics have already been used. Performing blood cultures during episodes of chills and fever, or conducting three consecutive cultures at 2-hour intervals upon initial diagnosis, increases the likelihood of successful pathogen identification. Simultaneous antimicrobial susceptibility testing for identified pathogens guides antibiotic selection.
Imaging Studies
Early in the disease (within 14 days), X-ray plain films often reveal no abnormalities. Characteristic X-ray findings include:
- Soft tissue swelling and shadowing.
- Irregular moth-eaten bone destruction, with obscured or missing trabeculae. Bone destruction can affect a large portion or entire diaphysis, potentially causing cortical disruption and pathological fractures.
- Periosteal reaction: Subperiosteal abscess stimulates the periosteum, producing lamellar, lace-like, or radiating patterns of dense shadows on the cortex.
CT scans help evaluate the extent and location of subperiosteal abscesses, soft tissue abscesses, and bone destruction.
MRI is effective in early detection of localized intraosseous inflammatory lesions and provides accurate delineation of lesion extent, edema severity, and abscess formation.
Localized Layer-by-Layer Aspiration
Aspiration is performed with a puncture needle containing an inner core, targeting the area of maximum tenderness. Slow insertion is combined with aspiration. If no fluid is obtained, the needle is advanced systematically until the periosteum and thin metaphyseal cortical bone are penetrated. Aspiration of purulent or hemorrhagic fluid warrants smears for analysis. Pus cells or bacteria in the smear confirm the diagnosis. Cultures and antimicrobial susceptibility testing should be performed on the aspirated fluid.
Diagnosis and Differential Diagnosis
Diagnostic Criteria
Diagnostic criteria include:
- Systemic signs of toxicity, such as chills, high fever, persistent localized pain, reluctance to move the affected limb, redness, swelling, increased skin temperature, and deep tenderness.
- Laboratory findings, including elevated white blood cell count, increased neutrophil ratio, elevated ESR, elevated CRP, and possible positive blood cultures for pathogens.
- Layered aspiration reveals purulent fluid and inflammatory exudates, with positive smear results for bacteria or pus cells.
- X-ray findings, such as bone destruction and periosteal reactions. However, X-ray abnormalities typically appear two weeks after onset and are not reliable for early diagnosis.
Key Differential Diagnoses
Acute Cellulitis and Deep Abscesses
Systemic symptoms differ. Acute osteomyelitis presents with severe toxic symptoms, whereas cellulitis and deep abscesses generally lack systemic symptoms.
The site of involvement differs. Acute osteomyelitis commonly affects the metaphysis, a less typical location for cellulitis or abscesses.
Physical findings differ. Acute osteomyelitis involves deep tenderness with initially minimal surface inflammation, whereas soft tissue infections exhibit evident local inflammatory signs. When differentiation is difficult, MRI may assist in diagnosis.
Osteosarcoma and Ewing's Sarcoma
Some malignant bone tumors present with fever and periosteal reactions. However, these conditions usually have a more gradual onset, with lesions primarily located in the diaphysis, particularly in Ewing's sarcoma. Visible engorgement of superficial vessels and palpable masses are typically identified. A biopsy may be required for definitive differentiation.
Treatment
Acute suppurative osteomyelitis requires prompt systemic and local treatment upon diagnosis to prevent progression to chronic osteomyelitis.
Systemic Treatment
This includes supportive therapy and antibiotic therapy. Systemic support aims to enhance immune function. Fresh blood or immunoglobulin may be administered in small, repeated doses, along with a high-protein, high-vitamin diet. Physical cooling methods may be utilized for high fever, with attention given to maintaining water-electrolyte balance and correcting acidosis.
Antibiotic treatment focuses on early, combined, adequate, and prolonged regimens. High doses of antibiotics are initiated immediately upon suspected diagnosis of acute suppurative osteomyelitis. Before pathogen identification and drug sensitivity results are available, combined antibiotics are used, typically one targeting Gram-positive cocci and another being a broad-spectrum antibiotic. Subsequent adjustment to sensitive antibiotics is guided by susceptibility test results. Treatment continues until symptoms and signs resolve, laboratory parameters normalize, and surgical drainage fluid appears clear.
Local Treatment
This includes immobilization of the affected limb and surgical intervention. Immobilization with a plaster splint or skin traction reduces inflammation, alleviates pain, and prevents pathologic fractures and joint contractures.
Surgical interventions serve the following purposes:
- Drain pus and mitigate symptoms of sepsis.
- Prevent the progression of acute osteomyelitis into chronic osteomyelitis.
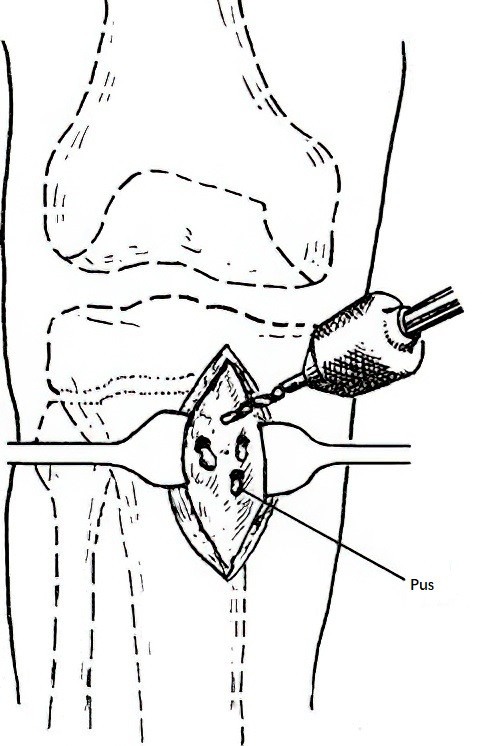
Figure 4 Schematic diagram of drilling and drainage of the proximal tibial metaphysis
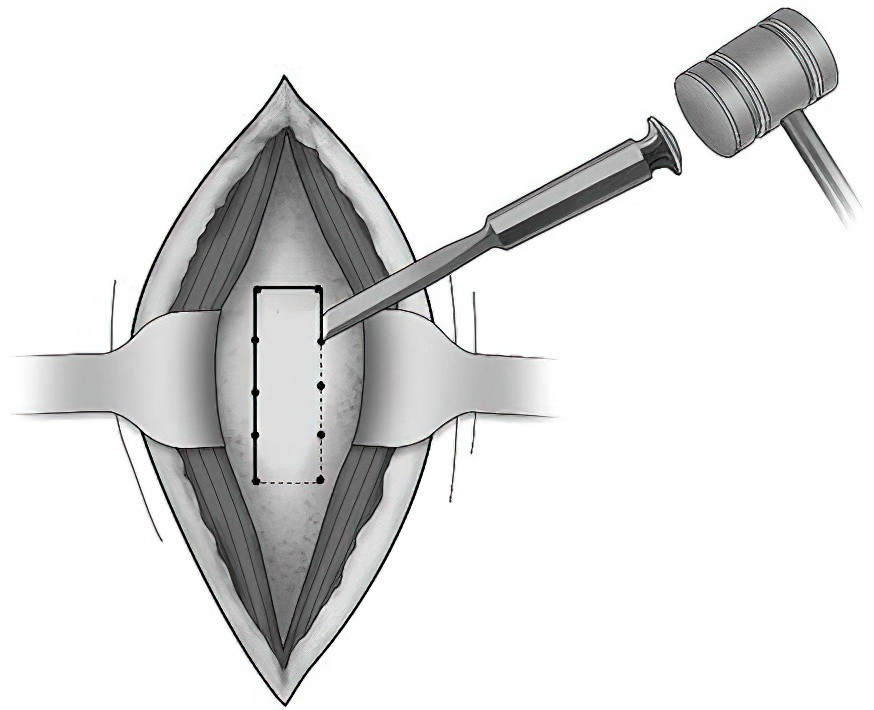
Figure 5 Schematic diagram of decompression and drainage via cortical fenestration
Early surgery is recommended. Techniques include drilling for drainage or creating a cortical “bone window” for decompression and drainage. A longitudinal incision is made at the point of maximum metaphyseal tenderness, with the periosteum incised to release subperiosteal abscesses if present. If no abscess is found, the periosteum on both sides is elevated (2 cm in each direction). Drilling multiple holes in the metaphysis, or using a bone chisel to connect these holes into a unified “bone window,” ensures adequate drainage. After thorough irrigation, both an irrigation catheter and a drainage catheter are placed for continuous washing and drainage. Sensitive antibiotics may be added to the irrigation solution.