Lumbar spondylolisthesis is the most common form of spinal spondylolisthesis. It refers to the anterior or posterior displacement of one vertebral body relative to an adjacent vertebral body.
Etiology
Based on the underlying causes, spondylolisthesis can be classified into dysplastic, isthmic, degenerative, traumatic, pathological, and iatrogenic types. Isthmic and degenerative spondylolisthesis are the most frequently observed in clinical practice.
Clinical Manifestations
Isthmic Spondylolisthesis
Initial symptoms are often mild, but persistent lower back pain or accompanying leg pain may develop later. Pain exacerbates with activity and improves with bed rest. Leg pain may radiate to the lower leg, dorsal foot, or lateral foot. Severe cases of spondylolisthesis may result in bilateral lower limb symptoms and bowel or bladder dysfunction.
On physical examination, increased lumbar lordosis and a palpable step-off sign between spinous processes may be observed. Lumbar forward flexion range is limited, and the straight-leg raise test may elicit a sensation of tightness in the popliteal region. If nerve root compression is present, the straight-leg raise test becomes positive. Diminished toe dorsiflexion strength and reduced or absent Achilles reflex may also be noted.
Degenerative Lumbar Spondylolisthesis
The incidence of degenerative lumbar spondylolisthesis increases with age. The L4–L5 level is the most commonly affected, followed by L3–L4 and L5–S1. Lumbar back pain results from lumbar instability, increased lumbar lordosis, and degenerative or bulging intervertebral discs stimulating the sinuvertebral nerve. When spondylolisthesis compresses the nerve roots, sciatica and symptoms resembling lumbar spinal stenosis, such as neurogenic claudication, may occur.
On examination, a clear step-off sign at the lumbar spinous processes may not be apparent. Associated scoliosis or kyphotic deformities may be seen. Lumbar flexion is typically normal, while extension is restricted. Neurological findings depend on the specific nerve root affected, presenting as pain or sensory disturbances in the respective innervation area, along with corresponding muscle weakness or reflex abnormalities.
Imaging Studies
Signs of Pars Interarticularis Fracture
Oblique X-rays of the lumbar spine (45-degree projection) depict characteristic features: the superior articular process resembles a "dog's ear," the transverse process resembles a "dog's head," the pedicle appears as the "dog's eye," the inferior articular process resembles the "dog's foreleg," and the pars interarticularis represents the "dog's neck." A defect or fracture in the pars interarticularis ("dog's neck") appears as a radiolucent gap.
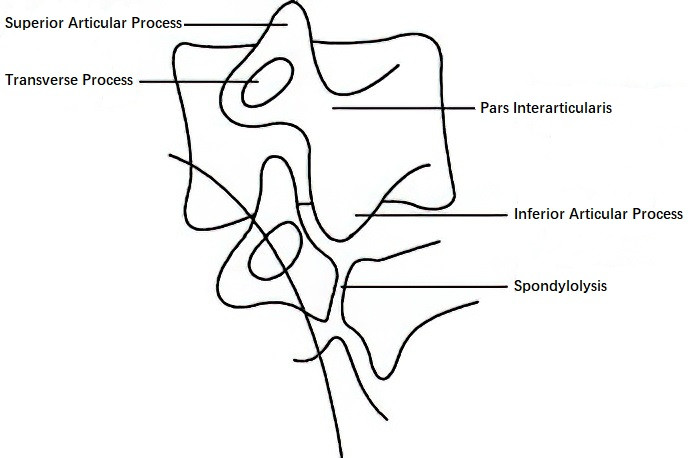
Figure 1 Illustration of pars interarticularis defects on an oblique X-ray of the lumbar spine
Meyerding Spondylolisthesis Grading
Lateral X-rays display anterior displacement of the upper vertebral body relative to the lower vertebral body. The superior edge of the lower vertebra is divided into four equal parts along the sagittal plane. Based on the degree of slippage, spondylolisthesis is graded as follows:
- Grade I: Slippage not exceeding 1/4 of the sagittal diameter of the vertebral body.
- Grade II: Slippage exceeding 1/4 but not exceeding 1/2.
- Grade III: Slippage exceeding 1/2 but not exceeding 3/4.
- Grade IV: Slippage exceeding 3/4 of the sagittal diameter.
CT and MRI Findings
CT imaging provides a detailed evaluation of the integrity of the pars interarticularis. MRI reveals information about dural sac and cauda equina compression.
Treatment
Conservative Treatment
For patients with mild symptoms, conservative management can be effective. This includes bed rest, nonsteroidal anti-inflammatory drugs (NSAIDs), traction, and bracing to protect the spine.
Surgical Treatment
Patients with significant low back or radiating leg pain, whether due to degenerative or isthmic spondylolisthesis, may require surgical intervention. Procedures include lumbar decompression, spondylolisthesis reduction, internal fixation, and spinal fusion. Although the extent of spondylolisthesis reduction remains controversial, the primary goal is effective decompression of the upper-level nerve roots affected by the spondylolisthesis gap.