Cervical disc herniation refers to a group of disorders that result from cervical disc degeneration, caused by minor trauma or no clear triggering factors, leading to disc protrusion and subsequent compression of the spinal cord or nerve roots.
Etiology and Pathology
When cervical disc degeneration occurs, partial damage or rupture of the posterior annulus fibrosus can happen. Under minor traumatic forces, overextension or overflexion of the cervical spine may cause the annulus fibrosus to sustain significant tensile stress, leading to its complete rupture. Nucleus pulposus material extrudes through the rupture into the spinal canal, compressing the spinal cord and nerve roots, producing corresponding symptoms and signs.
Clinical Manifestations
Cervical disc herniation commonly occurs in individuals aged 40–50, with the C5–6 and C4–5 levels being the most frequently affected. Affected individuals may have a history of neck pain or be asymptomatic until symptoms such as neck and shoulder pain or arm pain appear, either after minor trauma or without a clear trigger. Some may develop varying degrees of sensory or motor deficits in the limbs. Symptoms of cervical myelopathy or cervical nerve root compression occur depending on the degree and location of the herniation, with nerve root compression being more common than spinal cord compression or combined involvement.
When herniated disc material compresses the cervical nerve roots, patients experience neck and shoulder pain or radiating pain in the upper limb. The pain is often severe and radiates along the distribution of the nerve roots. In chronic cases, numbness predominates. Severe compression may manifest as an inability to raise the arm or hand weakness within a short duration. Examination may reveal restricted neck movement, an enforced cervical posture, or cervical stiffness. Sensory disturbances may occur in areas innervated by C2–T1 nerve roots, while muscle strength in the affected limb may decrease. Deep tendon reflexes may be diminished or absent, and Hoffmann's sign could be either negative or positive.
When herniated disc material compresses the spinal cord, patients may present with varying degrees of sensory, motor, or sphincter dysfunction in all four limbs. Other potential manifestations include paraplegia, quadriplegia, or conditions such as Brown-Séquard syndrome.
Imaging Examinations
Routine X-ray imaging includes anteroposterior, lateral, and oblique views of the cervical spine to assess alignment, changes in intervertebral disc height, alterations in the shape of the intervertebral foramina, and degenerative changes such as osteophyte formation. CT scanning can identify the type of disc herniation, the presence of osteophytes, or thickening, calcification, or ossification of the posterior longitudinal ligament or ligamentum flavum, along with hypertrophic changes in the facet joints and alterations in spinal canal morphology. MRI is key for the diagnosis of cervical disc herniation, as it provides detailed visualization of the cervical anatomical structures. T1- and T2-weighted images allow for the evaluation of the morphology of the herniated disc, spinal cord compression, and pathological changes such as spinal cord degeneration or edema.
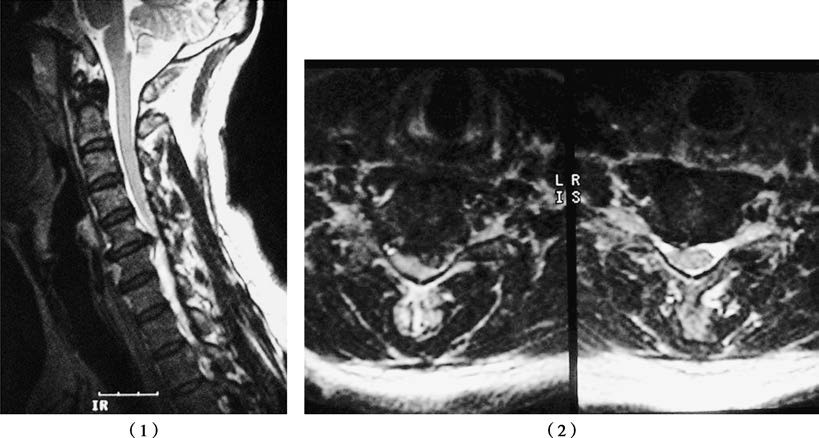
Figure 1 C5–C6 cervical disc herniation
The sagittal (1) and axial (2) MRI views demonstrate herniated disc material compressing the dural sac and spinal cord.
Diagnosis and Differential Diagnosis
A diagnosis can typically be established when clinical symptoms align with imaging findings in cases of classic cervical disc herniation. However, differential diagnosis is necessary to distinguish it from cervical spinal stenosis, intraspinal tumors, and shoulder-related conditions. Differences in clinical features and imaging findings, particularly MRI, provide critical evidence for differentiation.
Treatment
Treatment plans are based on the patient's clinical symptoms, physical signs, and imaging findings. For cases predominantly involving nerve root compression, non-surgical treatment is initially recommended. This approach includes adequate rest, bed rest, cervical traction, or physiotherapy, along with medications such as dehydrating agents, analgesics, and neurotrophic drugs. Surgical intervention is considered when non-surgical treatments are ineffective, symptoms worsen, or severe manifestations like muscle paralysis develop. Surgical options include discectomy to relieve compression on the nerve roots and spinal cord. The classic surgical technique is anterior cervical discectomy and fusion (ACDF). More recently, advancements in spinal endoscopic techniques have popularized posterior percutaneous endoscopic discectomy as a clinical option.