Osteonecrosis of the femoral head (ONFH) refers to a condition where the interruption or impairment of blood supply to the femoral head leads to the death of bone cells and bone marrow components. This results in necrosis of bone tissue and subsequent reparative processes, ultimately causing structural changes, collapse of the femoral head, and leading to hip pain and functional impairment. It is considered one of the common and challenging conditions in orthopedics to treat.
Etiology
The core pathological mechanism of ONFH is ischemia, driving subsequent pathological changes. The blood supply to the femoral head and neck comes from four primary sources: the medial and lateral circumflex femoral arteries, the obturator artery, and the nutrient artery of the femur. Most blood supply enters through the joint capsule, with a small portion passing through the round ligament of the femoral head. Among these, the medial circumflex femoral artery is the most critical.
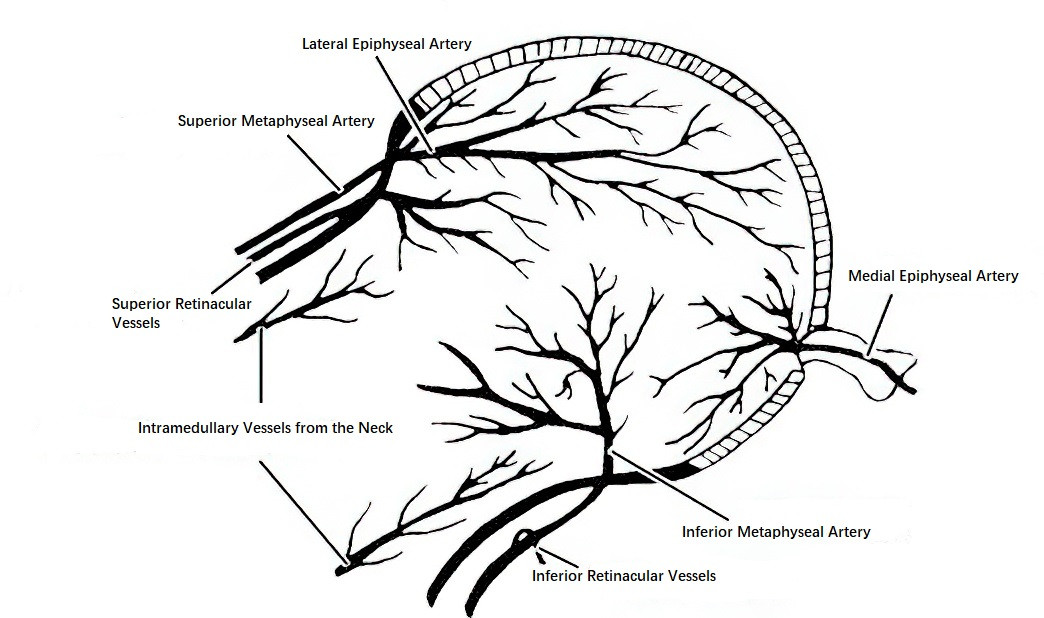
Figure 1 Blood supply of the femoral head and neck
The causes of ONFH are categorized into two main types: traumatic and non-traumatic.
Traumatic factors include femoral head or neck fractures, acetabular fractures, hip dislocations, and severe hip sprains or contusions (without fractures but with intra-articular hematomas).
Non-traumatic factors primarily include corticosteroid use, prolonged excessive alcohol consumption, decompression sickness, hemoglobinopathies (e.g., sickle cell anemia, hemoglobin C disease, thalassemia, sickle cell trait), autoimmune diseases, and idiopathic causes. Risk factors such as smoking, obesity, radiation therapy, and pregnancy are also associated with an increased likelihood of developing ONFH.
Pathology
From the perspective of pathological morphology, ONFH progresses through early, middle, and late stages of vascular changes.
Early Stage (Venous Stasis Stage)
During this stage, blood supply is obstructed, leading to early cellular necrosis. Over 50% of lacunae in trabecular bone lack viable osteocytes, extending to adjacent trabecular structures, with partial necrosis of the bone marrow. Exposure to pathogenic factors results in the differentiation of bone marrow stem cells into hypertrophic adipocytes. Microvascular changes include venous thrombosis, venous dilation, congestion of venous sinuses, and stromal edema, leading to venous stasis and high intraosseous pressure due to impaired venous return.
Middle Stage (Arterial Ischemia Stage)
Progressive venous thrombosis exacerbates vascular occlusion, leading to narrowing or thrombosis of arteries, which causes arterial insufficiency and ischemia. Subchondral fractures, expansion of the necrotic area, localized cystic degeneration, and partial collapse of the femoral head may occur. Reparative processes are initiated at this stage, with new blood vessels and fibrous tissue infiltrating the necrotic region to form granulation tissue.
Late Stage (Arterial Occlusion Stage)
Proliferation and thickening of arterial endothelium result in lumen narrowing and even complete occlusion. This stage features progressive worsening of femoral head collapse and the eventual development of osteoarthritis in the hip joint.
These pathological changes primarily describe non-traumatic ONFH. Traumatic ONFH often presents with immediate occlusion or disruption of arterial and venous blood flow at the onset of trauma, directly entering an ischemic state. Over time, pathohistological changes similar to the middle and later stages of vascular disruption may appear.
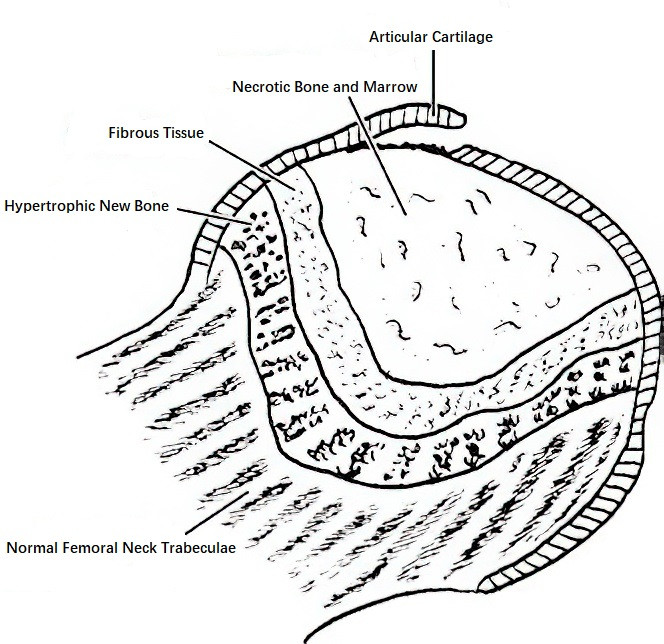
Figure 2 Coronal section of a necrotic femoral head
A sagittal cross-section through the femoral head reveals five distinct layers under the microscope: the articular cartilage layer, necrotic bone layer, granulation tissue layer, new bone layer, and normal tissue layer.
Clinical Presentation and Diagnosis
Clinical Presentation
Non-traumatic ONFH typically affects middle-aged males, with bilateral involvement in 50–80% of cases. In the early stage, patients often experience pain in the groin, buttock, or hip region, sometimes accompanied by knee pain. Pain episodes may occur intermittently and gradually worsen. For bilateral cases, alternating pain in both hips can occur. Early ONFH may remain asymptomatic and is often detected incidentally through X-ray imaging. Typical physical findings include deep tenderness in the groin area, sometimes radiating to the buttock or knee. A positive Patrick’s sign (figure 4 test) and tenderness in the adductor muscles may be observed. Hip joint movement is restricted, with limitations in internal rotation, flexion, and external rotation being most prominent.
The disease is closely associated with factors such as trauma, excessive alcohol intake, and corticosteroid use. A detailed history, including prior trauma, lifestyle habits, occupational exposures, past medical history, and medication usage, is essential for diagnosis.
Diagnosis
X-Ray Imaging
X-rays remain indispensable in diagnosing ONFH. Bone cell necrosis starts approximately 12 hours after the interruption of blood supply to the femoral head. However, changes in bone density on an X-ray may not become apparent until 2 months or more. Routine imaging should include anteroposterior and frog-leg lateral views, with the latter offering supplementary visualization of areas obscured in the standard anteroposterior view. Early radiographic findings include sclerosis, cystic changes, and the "crescent sign." Sclerosis demarcation at the boundary between necrotic and normal areas may also be seen. In the late stages, collapse of the femoral head disrupts its spherical morphology, with additional findings consistent with degenerative arthritis.
Computed Tomography (CT)
CT can detect early subtle bone changes and determine the presence of bone collapse. It can also delineate the extent of the lesion, aiding in the selection of treatment strategies. CT is more sensitive than plain X-rays for detecting femoral head osteonecrosis but is less sensitive than radionuclide scanning and magnetic resonance imaging (MRI).
Magnetic Resonance Imaging (MRI)
MRI is an effective non-invasive diagnostic method for early-stage lesions. Abnormal signals are typically observed in the anterosuperior portion of the femoral head. T1-weighted imaging (T1WI) typically shows a band-like low signal, while T2-weighted imaging (T2`WI) demonstrates a low signal or a "double-line sign," which consists of two parallel lines: an inner high signal and an outer low signal. The outer low-signal band represents sclerotic bone, while the inner high-signal band represents granulation and fibrous tissue repair. Associated findings may include bone marrow edema in the adjacent head and neck and joint effusion within the capsule.
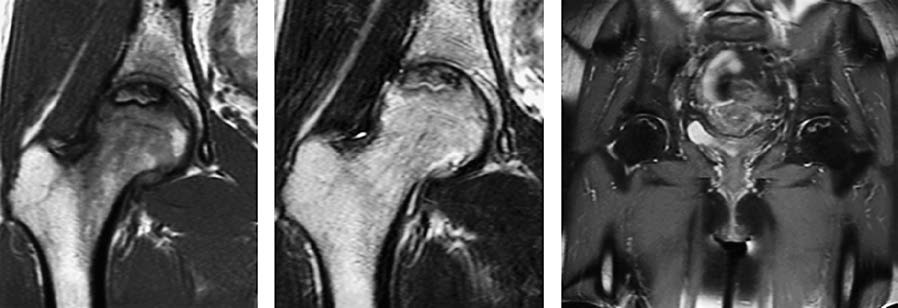
Figure 3 MRI manifestations of femoral head necrosis
Radionuclide Scanning
In the acute phase of femoral head osteonecrosis, bone scanning with agents such as 99mTc-MDP (technetium-labeled methylene diphosphonate) or 99mTc-DPD (technetium-labeled dicarboxypropane diphosphonate) reveals the necrotic area as a "cold zone." During the reparative phase, the scan may show a "hot zone" containing a central "cold zone," resembling a "doughnut-like" appearance. Single-photon emission computed tomography (SPECT) may enhance the diagnostic sensitivity of femoral head osteonecrosis. Positron emission tomography (PET) can potentially detect signs of osteonecrosis earlier than MRI and SPECT, as well as predict the progression of the disease.
Histological Examination
Although largely replaced by MRI, histological examination remains a reliable but invasive diagnostic method. Findings include the presence of more than 50% empty lacunae in trabecular bone, involving multiple adjacent trabeculae, along with evidence of bone marrow necrosis.
Clinical Staging
Several staging systems for femoral head osteonecrosis are currently in use. The 2019 staging system proposed by the Association Research Circulation Osseous (ARCO) categorizes the disease as follows:
- Stage 1: Normal plain X-rays, but MRI shows abnormal signals, with band-like low signals encircling the necrotic area. Bone scans reveal a "cold zone."
- Stage 2: Abnormal findings are observed on both plain X-rays and MRI. X-rays or CT reveal bone sclerosis, localized osteoporosis, or cystic changes without evidence of subchondral fractures, necrotic bone fractures, or flattening of the femoral head articular surface.
- Stage 3: X-rays or CT indicate subchondral fractures, necrotic bone fractures, and/or flattening of the femoral head articular surface. Based on the extent of femoral head collapse, this stage is further divided into Stage 3A (collapse ≤2 mm) and Stage 3B (collapse >2 mm).
- Stage 4: X-rays show signs of hip osteoarthritis, including joint space narrowing, acetabular changes, and joint destruction.
Treatment
Treatment strategies for femoral head osteonecrosis are determined based on factors such as MRI findings, the vascular changes involved, the stage of osteonecrosis, joint function, as well as the patient's age, occupation, and daily activity level.
Non-Surgical Treatment
Protective Weight-Bearing
The affected side should avoid weight-bearing. Walking with crutches or other assistive devices can help reduce the load on the femoral head. The use of wheelchairs, however, is not recommended.
Medications
Drugs that inhibit bone resorption and promote bone formation are commonly used, such as bisphosphonates. Other drugs include anticoagulants, lipid-lowering agents, vasodilators, and fibrinolytics.
Physical Therapy
Therapies such as extracorporeal shockwave therapy, electromagnetic field therapy, and hyperbaric oxygen therapy are some of the available options.
Surgical Treatment
Core Decompression Surgery
This reduces intraosseous pressure, alleviates pain, and improves venous outflow. This procedure facilitates vascular ingrowth.
Vascularized Bone Grafting
Vascularized iliac or fibular bone grafts are commonly used, combined with microsurgical techniques. This approach is suitable for patients with no or mild collapse of the femoral head.
Osteotomy
This procedure aims to shift the necrotic area away from the weight-bearing zone of the femoral head. Common techniques include intertrochanteric rotational osteotomy and its modifications.
Total Hip Arthroplasty (THA)
This is an option for patients with involvement of both the acetabulum and femoral head, accompanied by signs of osteoarthritis and significant impairment to quality of life.