Adhesive capsulitis, also known as frozen shoulder, periarthritis of the shoulder, or "fifty shoulder," is a condition characterized by stiffness and pain in the shoulder joint. It can occur as a primary (idiopathic) disease or in association with other conditions.
Etiology
Shoulder-Related Causes
Most cases occur around the age of 50, attributed to degenerative changes in soft tissues and a reduced ability to tolerate external forces.
Prolonged overactivity, poor posture, and repetitive strain often act as triggering factors for chronic injury.
Following upper limb injuries, prolonged shoulder immobilization may lead to secondary atrophy and adhesions of the surrounding tissues.
Acute trauma or overstretching of the shoulder, combined with improper treatment, can also contribute to the condition.
Extrinsic Factors
Conditions such as cervical spondylosis or diseases of the heart, lungs, or biliary system may cause referred shoulder pain. Chronic persistence of the primary disease can result in sustained shoulder muscle spasms, ischemia, and the development of inflammatory lesions, progressing to adhesive capsulitis.
Patients with diabetes are at significantly higher risk, with a prevalence rate of 10–20%. Adhesive capsulitis is also associated with thyroid diseases, prolonged immobility, stroke, and autoimmune disorders.
Pathology
Chronic injury and inflammation affect muscles, tendons, bursae, and the joint capsule. Proliferation of fibroblasts and myofibroblasts along with increased Type I and Type III collagen result in chronic fibrillation and fibrosis of the joint capsule. Additionally, synovial hyperemia and edema may eventually lead to adhesion and narrowing of the joint capsule. Thickening and contracture of the coracohumeral ligament into a band-like structure play a significant role in the limitation of external rotation.
Clinical Characteristics
Adhesive capsulitis is typically self-limiting and can resolve spontaneously over 6 to 24 months, although some patients may not regain normal shoulder function.
The condition primarily affects middle-aged and elderly individuals, with a higher prevalence in women than men and more frequent involvement of the left shoulder. Bilateral involvement may occur sequentially.
Both active and passive shoulder movements are restricted, with external rotation, abduction, and internal rotation with extension being the most affected. Localized shoulder pain develops early in the disease, with symptoms often related to specific activities or postures. Over time, the pain becomes more diffuse, spreading to the mid-upper arm and accompanied by increased limitation of shoulder motion. Attempts to forcefully increase the range of motion frequently elicit sharp, intense pain. In severe cases, activities such as combing hair or reaching behind the back become impossible. Nighttime disturbances, including waking due to shoulder movement during turning, are common. In early stages, distinct painful points may be identified, but as the disease progresses, the area of pain broadens.
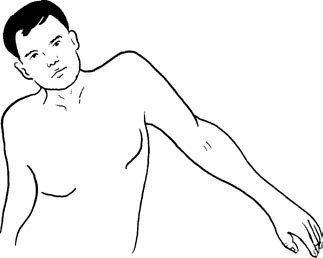
Figure 1 The abducted posture in adhesive capsulitis is often compensated for by contralateral trunk bending.
Imaging studies typically reveal normal shoulder structures on X-rays, though some patients may exhibit varying degrees of osteoporosis. MRI findings may include thickening of the joint capsule and potential bursitis with effusion. MRI plays an important role in differential diagnosis.
Differential Diagnosis
Rotator Cuff Injury
This affects individuals over the age of 60, presenting with shoulder and neck pain, along with weakness in the shoulder joint.
Passive range of motion remains largely normal.
A painful arc is observed.
Drop-arm test is positive.
Ultrasonography or MRI shows characteristic signs of rotator cuff tears.
Subacromial Impingement Syndrome
This presents with lateral shoulder pain, often worse at night.
Difficulty in abduction or elevation of the shoulder is present.
X-rays may reveal sclerosis or bone spur formation involving the acromion and the greater tuberosity of the humerus.
Ultrasonography or MRI excludes rotator cuff injury.
Shoulder Instability
A history of trauma, such as fractures or dislocations, is typically present.
Symptoms include peri-shoulder pain and weakness.
Imaging studies reveal partial defects involving the humeral head or glenoid.
Arthroscopy identifies signs of bone or joint capsule damage.
Cervical Spondylosis
Symptoms of nerve root irritation are often present.
Passive shoulder motion remains largely normal and pain-free.
Narrowing of the intervertebral foramina may be visualized on oblique X-rays.
Electromyographic studies suggest nerve root-related injury.
Other Causes
These conditions need to be differentiated:
- Shoulder pain following permanent pacemaker implantation.
- Dorsal scapular nerve entrapment syndrome.
- Pain associated with lateral clavicular fractures or use of clavicle hook plates.
- Inflammatory or neoplastic conditions of the thoracic cavity or the cervical-shoulder region.
Treatment
The primary goals include pain relief, restoration of functional motion, and prevention of muscle atrophy.
Early treatment modalities such as physiotherapy, acupuncture, and appropriate manual therapy can help improve symptoms.
Local injection of prednisolone acetate at the pain point can significantly alleviate pain.
Persistent pain, especially pain disrupting sleep, may be managed temporarily with nonsteroidal anti-inflammatory drugs (NSAIDs).
Active shoulder exercises are recommended on a daily basis regardless of disease duration or severity, while ensuring movements stay within a pain-free range.
For severe or refractory cases unresponsive to conservative treatments, adhesive release under anesthesia or arthroscopic intervention, followed by the injection of corticosteroids or hyaluronic acid, may achieve better outcomes.
For adhesive capsulitis secondary to extrinsic factors, treatment of the primary condition should accompany local therapeutic measures.