Stenosing tenosynovitis refers to a chronic aseptic inflammatory change in the tendon sheath caused by mechanical friction. The tendon sheath consists of two layers: an outer fibrous sheath and an inner synovial membrane, which is further divided into a parietal layer and a visceral layer. These layers form blind-ended sacs at both ends, containing a small amount of synovial fluid, which lubricates and facilitates tendon movement. Together with bone, the tendon sheath forms a "bone-fibrous tunnel" with minimal elasticity. The proximal or distal margins of the tendon sheath, especially at the level of the metacarpophalangeal joint, are relatively rigid, with thickening most prominent in an area known as the annular ligament. Prolonged or excessive friction along these rigid margins can cause inflammatory injury to both the tendons and tendon sheath. Tenosynovitis can occur in any limb tendon that passes through a "bone-fibrous tunnel," such as tenosynovitis of the long head of the biceps tendon, the extensor pollicis longus tendon, the extensor digitorum tendons, the fibularis longus and brevis tendons, as well as the flexor digitorum tendons, the flexor pollicis longus tendon, and the tendons of the abductor pollicis longus and extensor pollicis brevis. Among these, the final three are the most common and are therefore discussed in detail below.
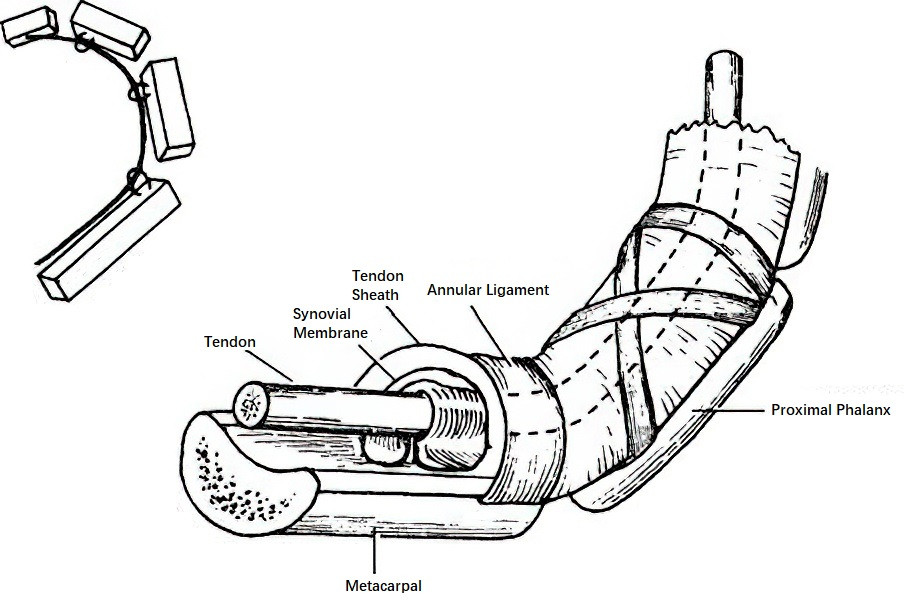
Figure 1 Schematic diagram of the bone-fibrous tunnel of the digital flexor tendon
Stenosing tenosynovitis of the hand and wrist is the most frequently observed form of this condition. In the fingers, it commonly presents as flexor tenosynovitis, often referred to as "trigger finger." In the thumb, it involves the flexor pollicis longus tendon and is referred to as "trigger thumb." In the wrist, it involves the abductor pollicis longus and extensor pollicis brevis tendons and is referred to as stenosing tenosynovitis of the radial styloid process or de Quervain's tenosynovitis.
Etiology
Repetitive quick hand or finger movements, such as knitting, practicing or performing on string instruments, as well as activities involving prolonged finger exertion, such as washing, writing, typing, or other computer tasks, represent primary causes of chronic strain leading to this condition. Congenital tendon abnormalities, underlying conditions such as rheumatoid arthritis, or generalized weakness following postpartum recovery or illness can increase susceptibility to stenosing tenosynovitis.
Pathology
Stenosing tenosynovitis is not limited to inflammatory injury of the tendon sheath. Both the tendon and the tendon sheath exhibit edema, hyperplasia, adhesion, and degeneration. Edema and hyperplasia of the tendon sheath progressively narrow the "bone-fibrous tunnel," compressing the already swollen tendon. The annular ligament area is particularly constricted and rigid, causing the swollen tendon to take on a "gourd-like" shape, which obstructs tendon gliding. Forced flexion or extension of the affected finger results in the enlarged gourd-shaped portion abruptly passing through the narrow annular ligament, producing snapping sensations, sounds, and pain. This phenomenon gives rise to the term "trigger finger."
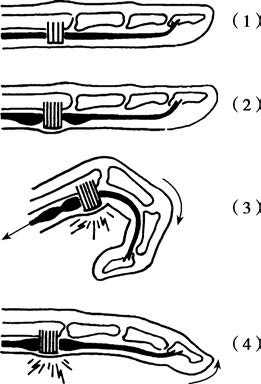
Figure 2 Mechanism of trigger finger
(1) Normal tendon and tendon sheath.
(2) Gourd-shaped tendon swelling and sheath thickening in disease.
(3) Snapping sensation during active finger flexion with the swollen portion forced through the narrowed tendon sheath.
(4) Similar snapping sensation during finger extension.
Clinical Manifestations
Trigger Finger and Trigger Thumb
The onset is gradual, initially presenting as stiffness and pain in the affected finger upon awakening, which resolves with slow movement. With disease progression, pronounced triggering and significant pain develop. In severe cases, the affected finger may remain flexed, with the patient reluctant to move it. Among the digits, the middle and ring fingers are most frequently affected, followed by the index and thumb, with the little finger being least affected. Patients often report pain near the proximal interphalangeal joint rather than the metacarpophalangeal joint. Physical examination typically identifies a small painful nodule at the level of the distal palmar crease, which moves up and down with the flexor tendon during finger movement. Snapping or triggering can often be observed and felt at this site.
Congenital flexor pollicis longus tenosynovitis in children is frequently bilateral. The condition manifests as triggering of the thumb during flexion or extension or as locking of the interphalangeal joint in the flexed position. A palpable painful nodule may be detected at the metacarpophalangeal joint. Observant caregivers often identify the condition within several months of birth, though some cases are only noticed at ages 3 to 4.
Stenosing Tenosynovitis of the Radial Styloid Process (de Quervain's Tenosynovitis)
This condition is characterized by progressive pain on the radial side of the wrist and weakness in gripping objects. Physical examination reveals localized tenderness over the radial styloid process or its distal aspect without signs of inflammation in the overlying skin. A painful nodule may occasionally be palpated. Pain exacerbation during the Finkelstein test, which involves ulnar deviation of the wrist while gripping a fist, suggests a positive result.

Figure 3 Finkelstein test (ulnar deviation of the wrist with the fist clenched)
Treatment
Conservative management typically includes adjustment of hand activities, splinting, and/or short-term use of NSAIDs. Patients with unresolved symptoms following conservative therapy may benefit from local corticosteroid injection. For those with severe symptoms or frequent triggering, corticosteroid injection may be considered at the initial visit. Injections must be performed accurately near the periosteum adjacent to the tendon sheath. Subcutaneous injection is ineffective and carries the risk of introducing the drug into the superficial branch of the radial artery, potentially leading to vasospasm or embolism in three radial-side digits and consequent fingertip necrosis.
Surgical release of the stenotic tendon sheath is considered if non-surgical treatment proves ineffective. Special care is required to retract the skin nerves and vessels on both sides of the incision, ensuring adequate exposure of the tendon sheath. Passive finger manipulation during the procedure typically reveals the enlarged nodule moving up and down through the tight stenotic sheath. Surgical release involves longitudinal incision of the thickened sheath along the tendon direction, ensuring sufficient length. The cut edges are trimmed by approximately 0.3 cm on both sides to fully relieve stenosis and prevent recurrence. Simple incision of the stenotic site may sometimes result in re-adhesion and symptom recurrence.
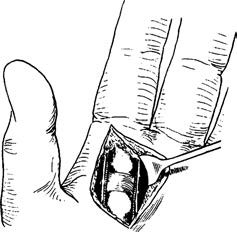
Figure 4 Intraoperative findings of trigger finger
Conservative treatment of congenital stenosing tenosynovitis in children is generally ineffective, and surgical intervention is usually required.