A bursa is a cushioning structure located in areas of frequent friction or significant pressure in the human body. It is a flattened connective tissue sac, with some bursae communicating with joint cavities while most exist independently. The bursa wall consists of two layers: the outer layer is composed of thin, dense fibrous connective tissue, while the inner layer comprises synovial endothelial cells that secrete synovial fluid. Under normal conditions, the bursa contains a small amount of synovial fluid. Due to the complex surrounding structures and frequent movement around joints, many bursae are located near large joints. These include "constant bursae," which are universally present, such as the prepatellar bursa, olecranon bursa, greater trochanteric bursa, and popliteal bursa. Other bursae develop secondarily to physiological or pathological needs; these are termed "secondary" or "accessory bursae," such as bursae over spinous processes in kyphosis, near the subcutaneous ends of internal fixation devices, or over the Achilles tendon. These secondary bursae may form as a result of increased local friction. Clinically, ischial tuberosity bursitis and big toe bursitis are commonly observed, especially in middle-aged and elderly women.
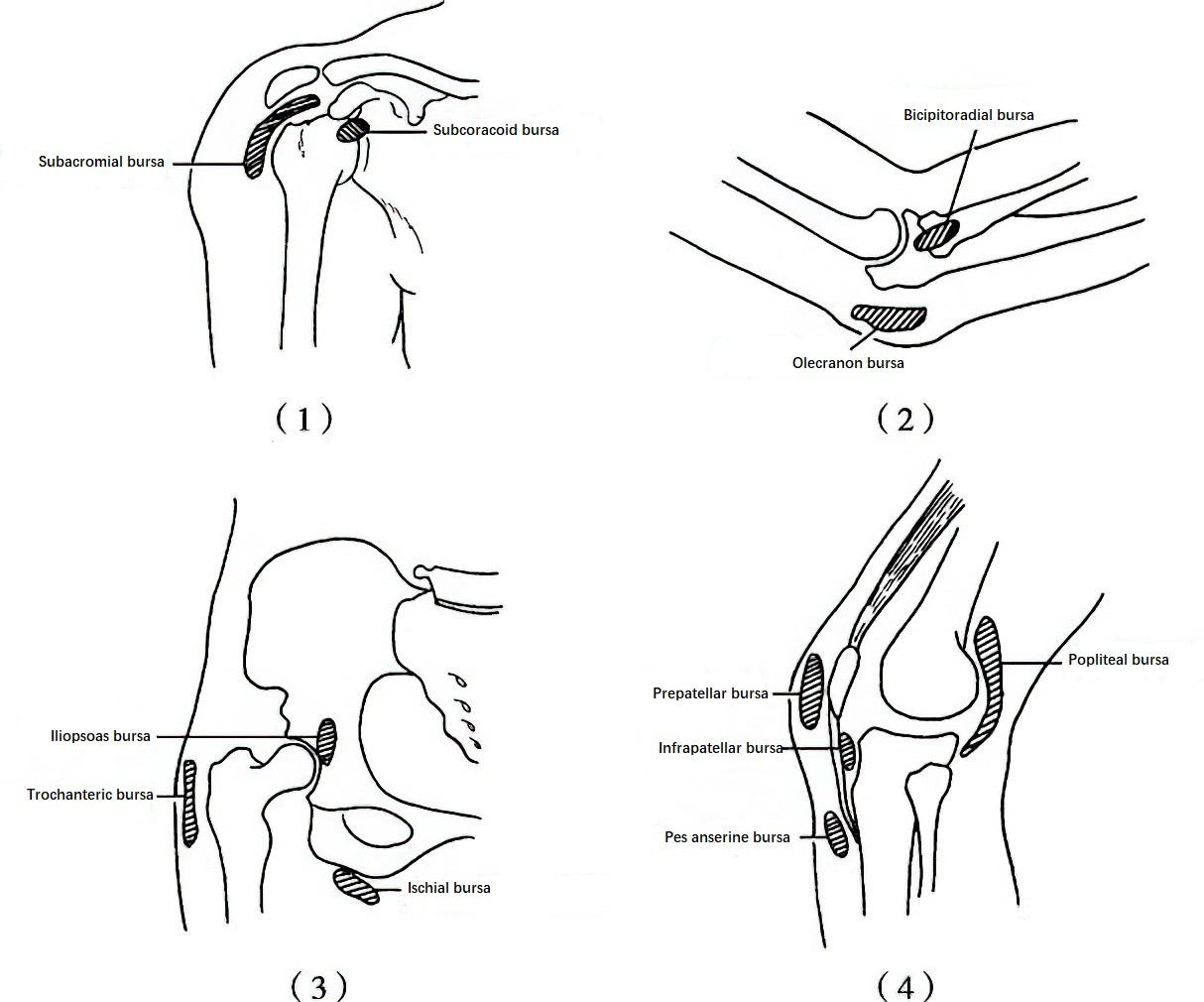
Figure 1 Common bursae around large joints
(1) Shoulder Bursae
(2) Elbow Bursae
(3) Hip Bursae
(4) Knee Bursae
Etiology and Pathology
Bursitis can be classified into several types based on etiology and characteristics, including traumatic bursitis, pyogenic bursitis, tuberculous bursitis, rheumatoid bursitis, gouty bursitis, and chemical bursitis.
Bursitis can present in acute or chronic forms, with chronic bursitis being more common. During the acute phase, the fluid accumulation in the bursa is typically hemorrhagic, later becoming yellowish. The chronic phase is characterized by mucoid fluid. In chronic bursitis, the bursa wall may show edema, thickening, or fibrosis, with synovial proliferation often appearing villous. In some cases, calcium deposition may occur within the bursa wall or tendons, potentially impairing joint mobility.
Bursitis is most likely to occur in areas where bones are prominent. Prolonged, repeated, concentrated, or moderately forceful friction and pressure represent the primary causes. Common examples include ischial tuberosity bursitis resulting from prolonged sitting on hard surfaces in frail elderly women, prepatellar bursitis in individuals who work in a kneeling position, and big toe bursitis due to prolonged wear of narrow, pointed shoes.
Clinical Manifestations
A rounded or oval-shaped swelling gradually develops over a joint or bony prominence without a clear cause and grows slowly, accompanied by tenderness. Bursitis in certain joint areas may be associated with partial functional impairment. For example, subacromial bursitis may present with joint pain, localized tenderness, and referred pain. In superficial locations, a clear boundary of the swelling can be palpated, along with a sense of fluctuation, without signs of bacterial skin infection. In deeper areas, boundaries may be unclear, and the condition may sometimes be mistaken for a solid tumor. Diagnostic differentiation can be achieved through ultrasonography or MRI.
If left untreated, bursitis in key joint locations may lead to gradual thickening and adhesion of the bursa wall, resulting in reduced joint mobility. In late stages, muscle atrophy around the joint may become apparent.
Treatment
Further friction and pressure should be avoided. Most cases resolve with appropriate joint immobilization and adjunctive physical therapy.
Initiation of treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) is commonly recommended for patients without contraindications. NSAIDs can also be used in conjunction with local injections, or as a standalone treatment when injections are contraindicated.
Aspiration of the bursal fluid followed by injection of prednisolone acetate and compression dressing may result in resolution of the condition.
Surgical excision of the bursa may be considered in cases unresponsive to conservative treatment, although the risk of recurrence exists.