Fractures in healthy bone tissue are typically caused by direct trauma. However, certain relatively fragile bone regions or areas with significant changes in bone structure are prone to stress concentration. When subjected to long-term, repetitive, and localized minor injuries, microfractures of the trabecular bone occur first, followed by repair. Continued exposure to external forces during the repair process impedes healing and increases bone resorption. This cycle repeats, and eventually, bone resorption exceeds repair, resulting in a complete fracture.
Fatigue fractures, also known as stress fractures, commonly occur in the diaphysis of the second metatarsal and ribs. Other potential sites include the third and fourth metatarsals, the distal fibula, the proximal tibia, and the distal femur. Approximately 80% of fatigue fractures are located in the feet.
Etiology
Major risk factors for fatigue fractures include a prior history of fatigue fractures, poor physical fitness, increased intensity or duration of physical activity, female gender with irregular menstruation, low BMI, insufficient calcium and vitamin D, poor bone health, anatomical abnormalities, and poor biomechanical alignment. Chronic repetitive injury represents the primary cause of fatigue fractures, although predisposing factors vary by location.
For example, congenital shortening or deformity of the first metatarsal shifts the weight-bearing focus from the head of the first metatarsal to that of the second metatarsal, which is structurally thinner and therefore more prone to fracture. This type of fracture is often observed in military recruits after training or long marches and is commonly referred to as a "march fracture." In elderly individuals with osteoporosis, repetitive vigorous coughing due to chronic bronchitis can cause intercostal muscle contractions, leading to fatigue fractures of the ribs.
Clinical Manifestations
Symptoms
Gradually worsening pain at the site of injury is the primary symptom. In early fatigue fractures of the first metatarsal, pain is often localized to the forefoot and becomes especially prominent during or after training.
Physical Examination
Localized tenderness and mild bony protrusion may be observed but without abnormal mobility. In a few cases, localized soft tissue swelling may also be present.
X-Ray Imaging
Plain X-rays often show no significant abnormalities within the initial 2–3 weeks after the onset of symptoms, and radiographic evidence of the fracture may only appear months later. Findings such as cortical thickening, sclerosis, or visible fracture lines may become apparent at that stage. In chronic cases, increased callus formation around the fracture site may be observed, with the fracture line appearing more distinct, along with sclerosis of the fracture ends. If clinical suspicion of a fatigue fracture persists despite negative X-ray findings, radionuclide bone scintigraphy or MRI may be considered as further diagnostic tools.
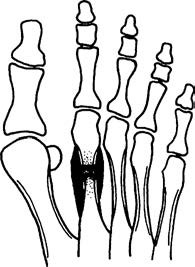
Figure 1 Fatigue fracture of the second metatarsal shaft.
MRI
MRI offers sensitivity comparable to bone scintigraphy but with greater specificity. It can detect enhanced edema signals at the fracture site in the early stages of development.
Treatment
The treatment of fatigue fractures follows principles similar to those for trauma-induced fractures. Due to the lack of significant displacement in most cases, treatment primarily involves firm external immobilization and proper functional rehabilitation exercises. Upon diagnosis, early intervention with 6–8 weeks of cast immobilization is recommended as delayed treatment increases the risk of ischemic necrosis and persistent disability. For late-presenting fatigue fractures with sclerosis at the fracture ends, bone healing may be more challenging. Timely and appropriate treatment can achieve good outcomes, but before resuming physical training, correction of incorrect movements or postures is essential to prevent reinjury. Reducing extended walking is also recommended.
In elderly individuals with rib fatigue fractures, management should include both anti-osteoporotic treatment and treatment of underlying conditions, such as chronic coughing.