Spinal cord injury is a severe complication of vertebral fractures. Displacement of vertebral bodies or intrusion of bone fragments into the spinal canal can lead to varying degrees of damage to the spinal cord or cauda equina. Injuries at the thoracolumbar level result in sensory and motor disturbances in the lower limbs, referred to as paraplegia. Injuries at the cervical level also cause neurological dysfunction in the upper limbs, resulting in quadriplegia.
Pathophysiology
Spinal Cord Concussion
After intense trauma, the spinal cord experiences excessive inhibition, leading to a temporary physiological suspension of its function. The structure of the spinal nerve cells remains intact, with no morphological changes observed.
Incomplete Spinal Cord Injury
Within 3 hours after injury, hemorrhage in the gray matter is minimal, and the white matter remains unchanged. Between 6 to 10 hours post-injury, hemorrhagic areas expand and neural tissue becomes edematous, which gradually subsides after 24 to 48 hours. The severity of incomplete spinal cord injuries varies; milder cases show only small central necrotic areas with most nerve fibers preserved, while more severe cases may exhibit necrotic and softened areas in the spinal cord center with only a small portion of nerve fibers remaining intact.
Complete Spinal Cord Injury
At 3 hours after injury, multiple hemorrhages are observed in the gray matter, while the white matter appears normal. At 6 hours, hemorrhage in the gray matter increases and white matter edema begins. After 12 hours, hemorrhagic lesions appear in the white matter, axonal degeneration begins, nerve cells in the gray matter start degenerating and dying, and axons in the white matter begin to degenerate. At 24 hours, necrosis is present in the center of the gray matter with multiple foci of axonal degeneration in the white matter. After 48 hours, the central gray matter becomes softened and white matter degeneration progresses. In cases of complete spinal cord injury, the pathological changes progress from central hemorrhage to widespread hemorrhagic edema and from central necrosis to extensive spinal cord necrosis, spanning up to 2–3 cm. In the late stage, the spinal cord is replaced by glial tissue.
Clinical Manifestations
Spinal Cord Concussion
Clinically, this condition presents as a complete or nearly complete loss of sensation, motor function, and reflexes below the level of injury. Sensory and motor functions generally begin to recover within hours to days, leaving no lasting neurological deficits.
Incomplete Spinal Cord Injury
Some sensory and motor functions are preserved below the level of injury. Incomplete spinal cord injuries include the following four types:
Anterior Spinal Cord Syndrome
Severe compression at the anterior cervical spinal cord, sometimes leading to occlusion of the anterior spinal artery, results in quadriplegia with the lower limbs more severely affected than the upper limbs. Position and deep sensation in the lower limbs and perineal area are typically preserved, and sometimes even superficial sensation remains. This syndrome is associated with the poorest prognosis among incomplete injuries.
Posterior Spinal Cord Syndrome
Motor function and pain, temperature, and touch sensations remain intact below the lesion level, while deep sensation is partially or completely lost.
Central Cord Syndrome
This commonly occurs with hyperextension injuries of the cervical spine. The central spinal cord conduction tracts are affected, resulting in quadriplegia with greater involvement of the upper limbs than the lower limbs. No sensory dissociation is observed.
Brown-Séquard Syndrome (Hemisection of the Spinal Cord)
Below the level of injury, motor function and deep sensation are lost on the same side as the injury, while pain and temperature sensation are lost on the opposite side.
Complete Spinal Cord Injury
In cases of complete transverse spinal cord damage, spinal shock initially presents as flaccid paralysis below the level of injury, including complete loss of sensory and motor functions as well as reflexes in the lowest sacral segments. Perianal sensation and sphincter contractions are absent. If motor and sensory function do not return after the shock phase ends, the injury is classified as complete. Over 2 to 4 weeks, the condition transitions into spastic paralysis characterized by increased muscle tone, exaggerated tendon reflexes, and pathological signs of corticospinal tract involvement. Thoracic spinal cord injuries result in paraplegia, while cervical injuries cause quadriplegia. Injuries to the upper cervical spine lead to spastic quadriplegia, while lower cervical injuries cause flaccid paralysis in the upper limbs (due to damage to the cervical enlargement and nerve roots) and spastic paralysis in the lower limbs.
Conus Medullaris Injury
The spinal cord in a normal person terminates at the lower edge of the L1 vertebral body. Therefore, fractures of T12 or L1 may cause injury to the conus medullaris, resulting in sensory loss in the perineal (saddle) region, loss of sphincter control leading to incontinence and sexual dysfunction, while sensory and motor functions in both lower limbs are typically preserved.
Cauda Equina Injury
The cauda equina originates from the sacral spinal cord at the L2 level and typically ends at the lower edge of the S1 vertebra. Complete cauda equina injuries are rare. This condition presents as flaccid paralysis below the level of injury, with impairments in sensory and motor functions as well as sexual function. Sphincter control is lost, muscle tone is decreased, and tendon reflexes are absent. No pathological signs of corticospinal tract involvement are present.
Assessment of Spinal Cord Injury Severity
The classification of spinal cord injury severity serves as an observational metric for understanding the natural progression of the injury and for comparing treatment outcomes. The grading is based on clinical presentations of spinal cord injuries, with the American Spinal Injury Association (ASIA) Impairment Scale being one of the most commonly used evaluation systems.
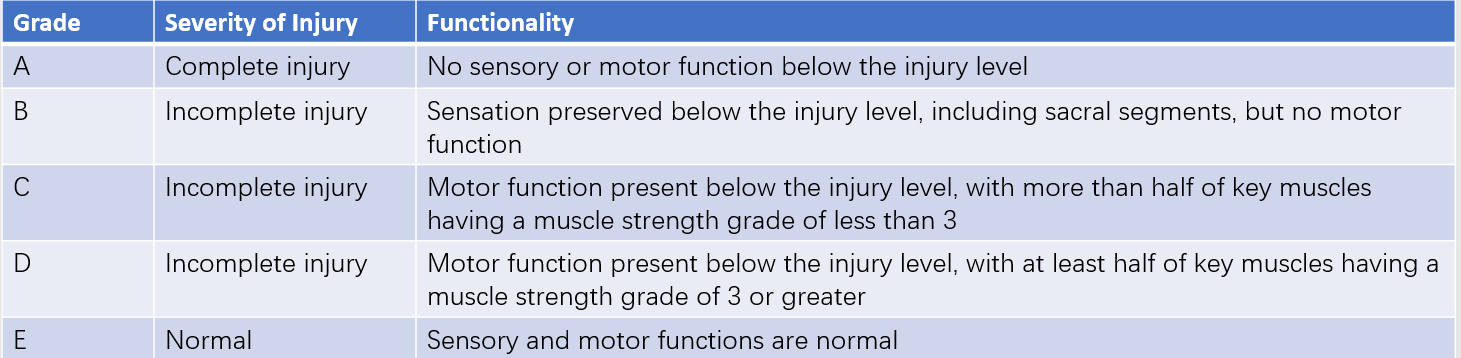
Table 1 ASIA impairment scale for spinal cord function
Imaging Examinations
X-ray and CT scans are the most routine imaging techniques used for spinal cord injury. They help detect spinal fractures or dislocations at the site of injury. In cases where disc and ligament structures are damaged but no clear abnormalities are visible on X-rays or CT scans, the condition may be referred to as spinal cord injury without radiographic abnormality (SCIWORA), which is more commonly observed in cervical spine trauma.
MRI scans may reveal changes associated with spinal cord damage. MRI allows for assessment of spinal cord compression severity, as well as signal intensity, the extent of signal changes, and spinal cord atrophy.
Electrophysiological Examinations
Somatosensory evoked potential (SEP) and motor evoked potential (MEP) tests are used to evaluate spinal cord function. SEP reflects the functionality of the sensory pathways in the spinal cord, while MEP assesses the functionality of the corticospinal motor pathways. Neither signal can be detected in cases of complete paraplegia.
Complications
Respiratory Failure and Pulmonary Infections
These are severe complications associated with cervical spinal cord injury. Following cervical spinal cord injury, intercostal muscles become completely paralyzed, leaving diaphragmatic breathing controlled by the phrenic nerve as the sole means of respiration. The phrenic nerve originates from C3–C5, with C4 being the primary component. Injuries to C1 and C2 often result in immediate death at the scene, while C3 and C4 injuries frequently lead to early death due to respiratory failure caused by impaired phrenic nerve function. Even injuries at C4 or below may result in respiratory dysfunction due to spinal cord edema extending upward to affect respiratory centers. Only injuries to the lower cervical spine preserve diaphragmatic breathing.
Weakness in the respiratory muscles increases airway resistance, making it difficult to clear secretions, which can lead to aspiration pneumonia or death from airway obstruction. Tracheostomy increases survival rates by reducing dead space in the airway, enabling clearance of secretions, providing mechanical ventilation, and allowing for drug administration via the trachea. However, tracheostomy increases caregiving challenges, and there is no consensus on the optimal timing for this procedure. Tracheostomy is generally indicated in cases such as:
- Upper cervical spine injury;
- Onset of respiratory failure;
- Presence of airway infection and difficulty in clearing secretions;
- Existing respiratory obstruction.
-
Appropriate antibiotics and regular repositioning with percussion therapy can help control lung infections.
Genitourinary Infections and Calculi
Loss of sphincter function causes the patient to experience urinary retention, requiring long-term urinary catheterization, which increases the risk of urinary tract infections and stones. Preventative measures include:
- Starting regular catheter clamping 2–3 weeks after the injury, massaging the bladder area to void urine, and training for a reflex bladder to allow early removal of the catheter;
- Teaching the patient to perform intermittent catheterization under sterile conditions;
- Performing permanent cystostomy in cases of long-term catheterization with uncontrolled genitourinary infections;
- After 4–6 months, once the injured site stabilizes, reconstructing an artificial somatic-autonomic reflex arc below the injury level to regain bladder control, improving micturition and defecation functions as well as partial sexual function recovery in some cases. Adequate hydration reduces the risk of urinary stones, and antibiotics are used in cases of infection.
Pressure Ulcers
Prolonged bed rest in paraplegic patients, combined with loss of skin sensation, leads to neurotrophic changes in areas of skin over bony prominences, resulting in necrosis, referred to as pressure ulcers. The most common sites include the sacrum, greater trochanter, iliac crest, and heels. Preventative and treatment steps include:
- Using an air cushion mattress and maintaining clean and dry skin;
- Repositioning every 2–3 hours;
- Cleaning bony prominences daily with 50% ethanol and massaging with talcum powder;
- Using infrared light for superficial pressure ulcers, while avoiding secondary burns;
- Removing necrotic tissue and frequently changing dressings for deep pressure ulcers;
- Controlling inflammation and employing skin grafting or flap techniques when granulation tissue is stable.
Thermoregulation Disorders
Cervical spinal cord injuries result in autonomic nervous system dysfunction, impairing the ability of skin below the injury level to sweat and adapt to temperature changes. This can lead to high fevers exceeding 40°C. Management includes:
- Placing patients in an air-conditioned room;
- Applying physical cooling methods such as ice packs, ice water enemas, or ethanol sponge baths;
- Administering medications such as intravenous fluids and hypothermic agents.
Treatment Principles
Non-Surgical Treatment
The period within 6 hours after injury is critical, and the first 24 hours after injury is considered the acute phase. Early treatment during this period is important.
Pharmacological Treatment
Methylprednisolone pulse therapy can be a treatment option for individuals injured within 8 hours. The dosage involves administering an initial dose of 30 mg per kilogram of body weight via intravenous injection over 15 minutes, followed by a 45-minute break, and then continuous intravenous infusion at a rate of 5.4 mg/(kg·h) for the subsequent 23 hours. The mechanism of action of high-dose methylprednisolone lies in its ability to inhibit lipid peroxidation and stabilize cell membranes, thereby reducing post-trauma nerve cell degeneration, alleviating tissue edema, improving spinal cord blood flow, and preventing the worsening of spinal cord ischemia. Additional pharmaceutical options include free radical scavengers, drugs that improve microcirculation, and excitatory amino acid receptor antagonists.
Hyperbaric Oxygen Therapy:
Animal studies indicate that hyperbaric oxygen therapy produces optimal results when administered within 2 hours after injury, although this timeframe is generally not feasible for clinical cases. Based on clinical experience, satisfactory outcomes are achievable when therapy is utilized within 4 to 6 hours post-injury.
Comprehensive Therapeutic Measures:
These measures include rehabilitation training, physical therapy, psychological counseling, and nutritional support.
Surgical Treatment
Surgery aims to relieve spinal cord compression and restore spinal stability but does not yet enable the recovery of function in damaged spinal cord tissues. The surgical approach and method depend on the type of fracture and the location of the compressive structures.
Indications for surgery include:
- Spinal fractures with facet joint interlocking;
- Unsatisfactory reduction of spinal fractures or persistent spinal instability;
- Imaging evidence of bone fragments protruding into the spinal canal and compressing the spinal cord;
- Progressive ascent of the paraplegia level, suggesting active bleeding within the spinal canal.