Spinal fractures include fractures of the cervical, thoracic, thoracolumbar, and lumbar vertebrae. These account for approximately 5–6% of all fractures in the body, with thoracolumbar fractures being the most common. Spinal fractures can be accompanied by spinal cord or cauda equina injuries, potentially leading to severe disability or even life-threatening conditions. The spine consists of 26 vertebrae (7 cervical, 12 thoracic, 5 lumbar, 1 sacral, and 1 coccygeal) connected by ligaments, facet joints, and intervertebral discs. Each vertebra comprises a vertebral body and associated structures. Anatomically and functionally, the spine is divided into anterior, middle, and posterior columns. The middle and posterior columns form the spinal canal, which houses the spinal cord and cauda equina. Injuries to these regions may involve the nervous system, particularly in cases of middle column injuries where bone fragments and nucleus pulposus material can protrude into the spinal canal and damage the spinal cord or nerves. The thoracolumbar region (T10–L2) is situated at the junction of the major physiological curves of the spine, making it a stress concentration point and a common site for fractures.
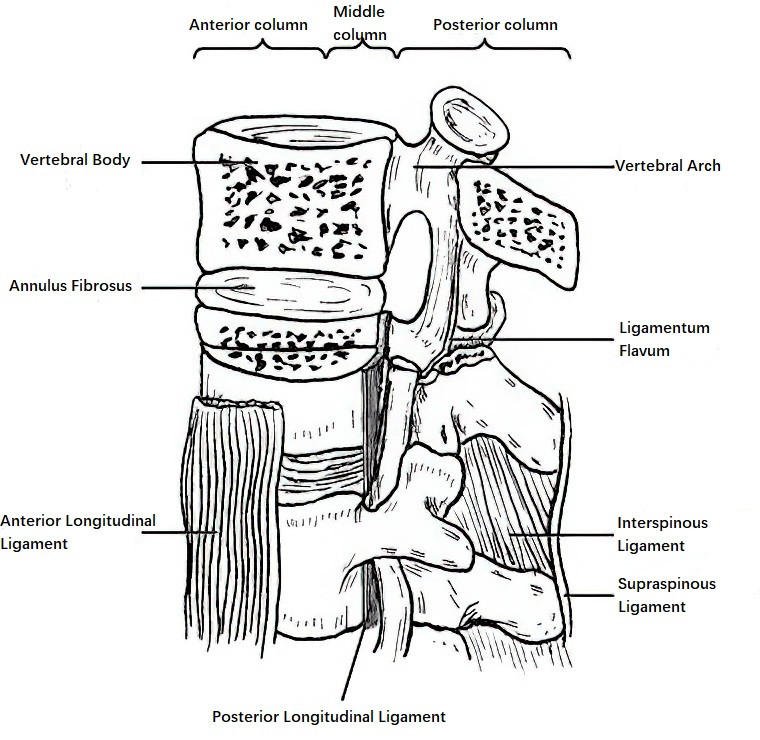
Figure 1 Anatomical structure and three-column model of the thoracolumbar spine
Anterior Column: Includes the anterior two-thirds of the vertebral body, the anterior portion of the annulus fibrosus, and the anterior longitudinal ligament.
Middle Column: Includes the posterior one-third of the vertebral body, the posterior portion of the annulus fibrosus, and the posterior longitudinal ligament.
Posterior Column: Includes the vertebral arch, posterior joint capsule, ligamentum flavum, supraspinous ligament, and interspinous ligament.
Classification
Classification of Cervical Spine Fractures
Cervical spine fractures are classified based on the position of the cervical spine (flexion, upright, or extension) at the time of injury into four types:
Flexion-Type Injuries
These injuries occur when violence impacts the cervical spine in a flexed position, causing compression of the anterior column and stretching injuries to the posterior column. Common examples include:
Compression Fractures
These are relatively common. Lateral X-rays typically reveal a wedge deformity at the anterior margin of the vertebral body or compression of the upper endplate. These fractures are more frequently observed in individuals with osteoporosis.
Fracture-Dislocations
Excessive flexion causes rupture of the posterior longitudinal ligament, and the force leads to the dislocated vertebral body’s inferior articular process moving anteriorly past the superior articular process of the vertebra below. This is referred to as "facet joint interlocking." With unilateral interlocking, the degree of displacement does not exceed one-quarter of the anteroposterior diameter of the vertebral body; with bilateral interlocking, displacement exceeds one-half of this diameter. Most cases in this group are associated with spinal cord injuries, and fractures of the articular processes may also occur.
Vertical Compression Injuries
These injuries arise when vertical stress impacts the cervical spine in an upright position without significant flexion or extension, such as being hit by falling objects or during high-diving incidents.
Jefferson Fractures
These fractures involve bilateral fractures of the anterior and posterior arches of the atlas (C1). On frontal X-rays, lateral displacement of the C1 lateral masses can be observed. CT scans provide detailed visualization of the fracture lines, number of fragments, and extent of displacement, while MRI assessments can reveal potential spinal cord injuries.
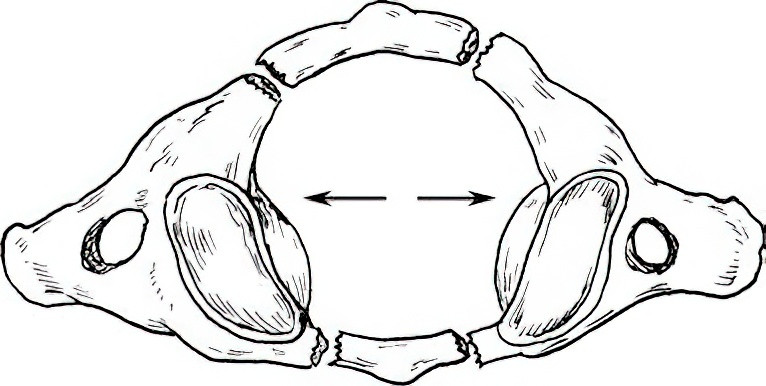
Figure 2 Jefferson fracture
Burst Fractures
These are comminuted fractures of the lower cervical vertebrae (C3–C7), most commonly C5 and C6. Bone fragments may intrude into the spinal canal to varying degrees, with quadriplegia occurring in up to 80% of cases.
Hyperextension Injuries
Hyperextension Without Fracture-Dislocation
These injuries often occur when the patient falls and lands on the forehead, causing hyperextension of the neck, which compresses the spinal cord. Such cases often involve pre-existing cervical spinal stenosis. They can also occur during high-speed driving accidents due to abrupt braking or collisions, where inertial forces cause the head to hyperextend followed by hyperflexion, resulting in "whiplash injuries." Pathological changes include rupture of the anterior longitudinal ligament, horizontal tears of the intervertebral disc, avulsion fractures of the anterior inferior vertebral margin of the upper vertebra, and rupture of the posterior longitudinal ligament. As the cervical spine translates posteriorly, the spinal cord becomes pinched between the folded ligamentum flavum and intervertebral disc, leading to central spinal cord damage.
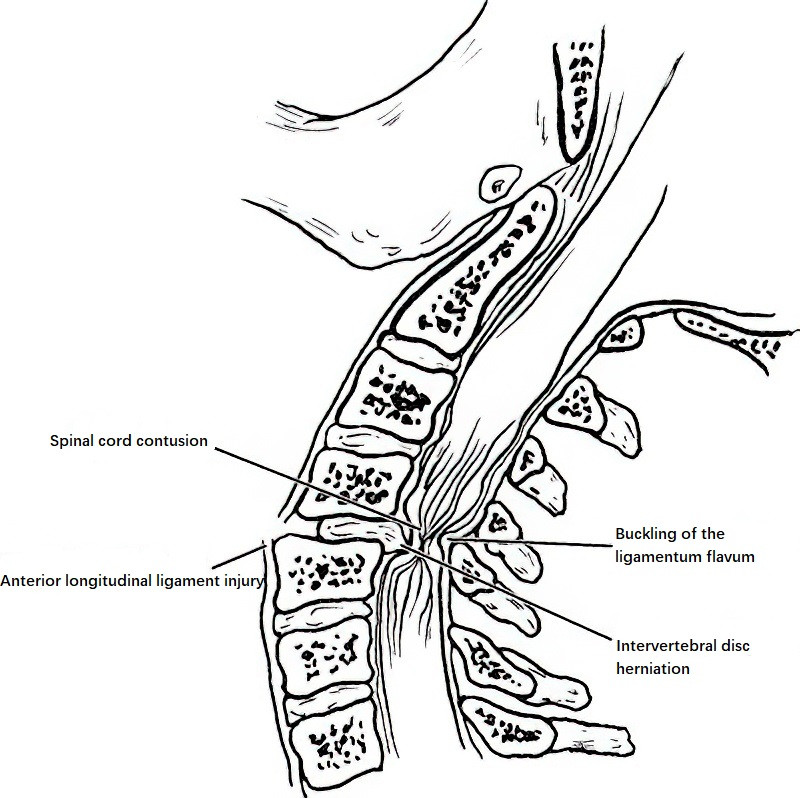
Figure 3 Spinal cord injury caused by hyperextension of the cervical spine
Axis (C2) Pedicle Fractures
These injuries result from force applied to the chin causing hyperextension of the cervical spine. Shearing forces in the posterior segment of the axis lead to fractures of the C2 pedicles. Historically, this injury was common in hanging victims and is thus also referred to as a "hangman’s fracture." Today, it is more commonly seen in motor vehicle accidents.
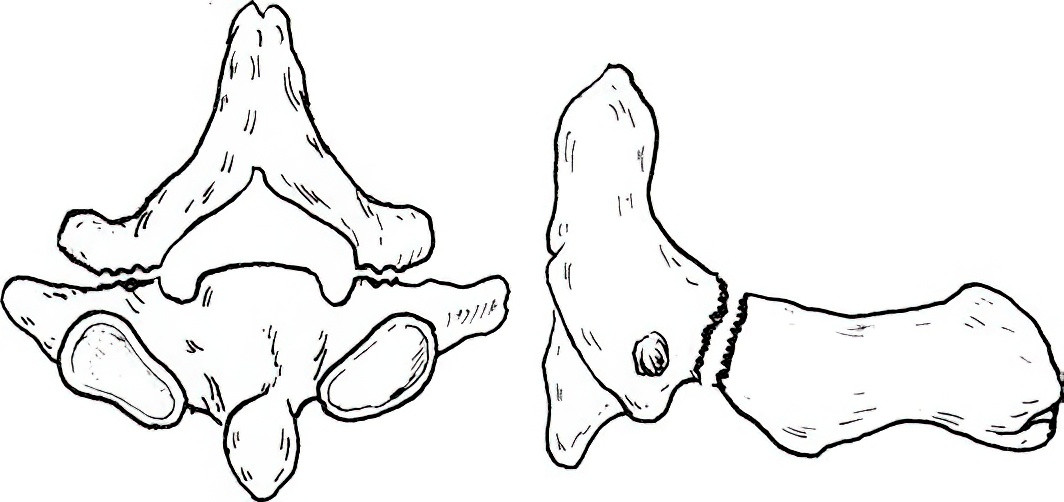
Figure 4 Axis pedicle fracture (hangman’s fracture)
Odontoid Process Fractures
The mechanisms causing fractures of the odontoid process remain unclear. Trauma may originate from horizontal forces or involve a combination of forces. Odontoid fractures are classified into three types:
- Type I: Avulsion fractures at the tip of the odontoid process. These fractures are stable, have few complications, and generally result in a favorable prognosis.
- Type II: Fractures at the base of the odontoid process, located above the body of the axis. These fractures are the most common, but the poor blood supply in this region leads to a non-union rate as high as 70%, often necessitating surgical intervention.
- Type III: Fractures that extend into the upper body of the axis and may involve one or both superior articular processes of the axis. These fractures are more stable, have good blood supply, a high union rate, and a favorable prognosis.
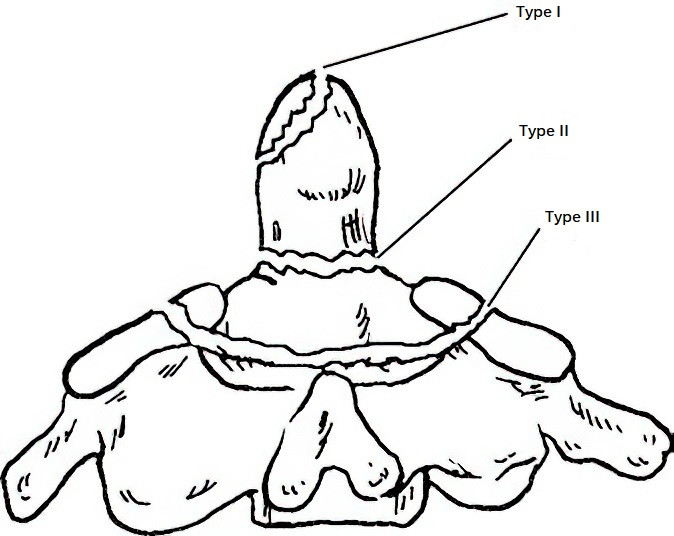
Figure 5 Classification of odontoid fractures
Classification of Thoracolumbar Spine Fractures
Classification Based on Fracture Stability
Stable Fractures
This category includes mild to moderate compression fractures with an intact posterior column, as well as isolated fractures of transverse processes, spinous processes, and laminae.
Unstable Fractures
These include:
- Fractures involving two of the three spinal columns.
- Burst fractures, where middle column injuries result in posterior vertebral fragments protruding into the spinal canal, with the potential for causing neurological damage.
- Fracture-dislocations involving anterior, middle, and posterior columns, often accompanied by symptoms of neurological injury.
Classification Based on Fracture Morphology
Compression Fractures
These are characterized by wedge-shaped compression of the anterior portion of the vertebral body. The degree of compression is calculated as the ratio of the vertebral body’s anterior height to its posterior height on lateral X-rays. These are generally stable fractures. Patients with osteoporosis may sustain compression fractures of the thoracolumbar spine from minor trauma.
Burst Fractures
These are comminuted fractures of the vertebral body where fragments are displaced outward in multiple directions. Posterior displacement of fragments can compress the spinal cord and nerves. X-rays and CT scans typically reveal an increased anteroposterior and transverse diameter of the vertebral body, widening of the pedicle distance, and reduced vertebral height.
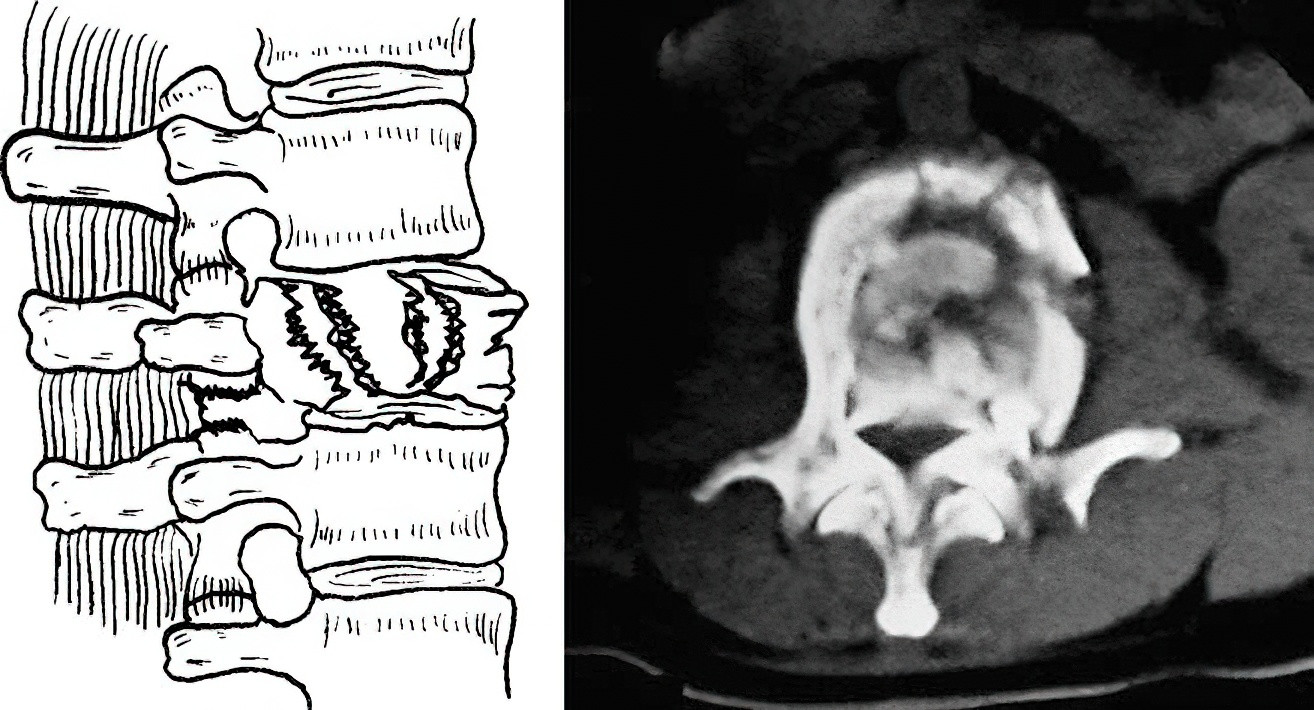
Figure 6 Burst fracture
Chance Fractures
These fractures involve horizontal breaks through the vertebral body, laminae, and spinous processes, or injury to the anterior and posterior longitudinal ligaments, intervertebral discs, and posterior ligament complex.
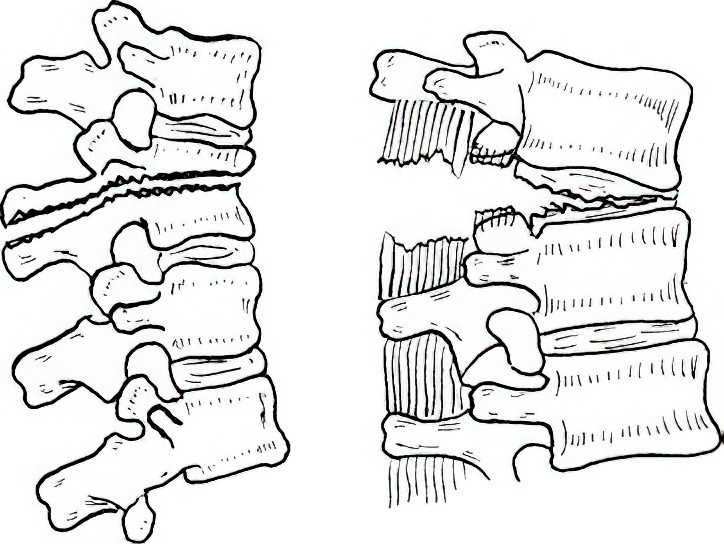
Figure 7 Chance fracture
Fracture-Dislocations
These involve fractures of all three spinal columns, with potential anterior, posterior, or lateral displacement of the vertebral body. These fractures may also involve dislocations or fractures of the facet joints.
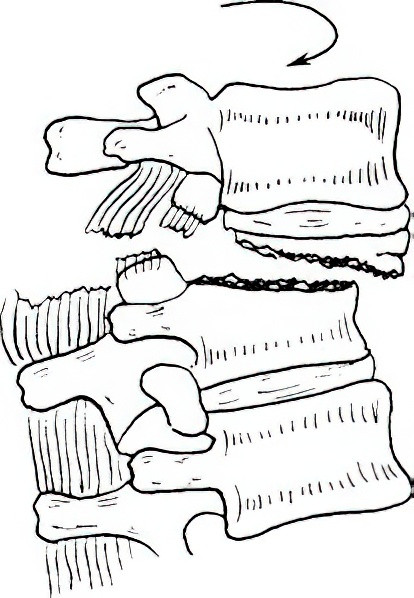
Figure 8 Fracture-Dislocation
Clinical Presentation
History
Trauma History
Most patients report significant trauma, such as motor vehicle accidents, falls from heights, or being struck by heavy objects. A detailed account of the time, mechanism, posture during injury, and limb activity after the injury is important.
Main Symptoms
These include:
- Localized pain.
- Difficulty standing or turning over in bed.
- Abdominal pain or distension, or even symptoms of intestinal paralysis due to retroperitoneal hematoma irritation.
- Paralysis may present as sensory and motor dysfunction in the limbs or loss of bladder and bowel control.
Associated Injuries
Attention should be paid to possible concomitant injuries to the head, chest, abdomen, and pelvic organs.
Physical Examination
Posture
Observations include the patient’s ability to stand or walk and whether they adopt a fixed (forced) posture.
Tenderness
Localized tenderness in the midline, often with swelling and significant pain upon palpation or percussion of the spinous processes, suggests injury to the posterior column.
Deformity
Thoracolumbar spine fractures often present with visible or palpable kyphotic deformities.
Sensory Examination: Pain, touch, and temperature sensations in the trunk and limbs should be assessed and recorded as "normal," "reduced," "absent," or "hypersensitive." Perineal sensation should also be evaluated.
Muscle Strength
Muscle strength is graded on a six-point scale from 0 to 5.
Reflexes
Knee and ankle reflexes, pathological reflexes, anal reflex, and bulbocavernosus reflex shoulde be assessed.
Imaging Studies
X-rays
Frontal and lateral X-rays of the affected area should be performed. Additional oblique or open-mouth views may be needed in specific cases.
CT Scans
CT imaging of the affected area, along with three-dimensional reconstruction, provides more detail. Whole-spine CT with 3D reconstruction can be performed if necessary.
MRI
Magnetic resonance imaging is recommended when there is suspicion of spinal cord or nerve damage, or injury to intervertebral discs and ligaments.
Diagnosis
The diagnosis is typically based on the trauma history, physical examination, and imaging studies. It should include the etiology (traumatic or pathological), fracture location, and fracture type.
Emergency Transport
Transport methods for spinal fracture patients from the injury site to the hospital are critically important. Carrying methods that involve lifting by the head and feet or cradling can be dangerous, as these may increase spinal flexion and risk forcing bone fragments into the spinal canal, exacerbating spinal cord injuries. Proper transport requires the use of a stretcher, wooden board, or door panel. The patient’s legs should first be straightened, and the stretcher positioned beside them. Caregivers can lift the patient onto the stretcher while maintaining a flat position or use a rolling technique to move the patient as a single, straight unit onto the stretcher. Regardless of the method used, cervical spine stability must be maintained to avoid worsening cervical spinal cord injuries.
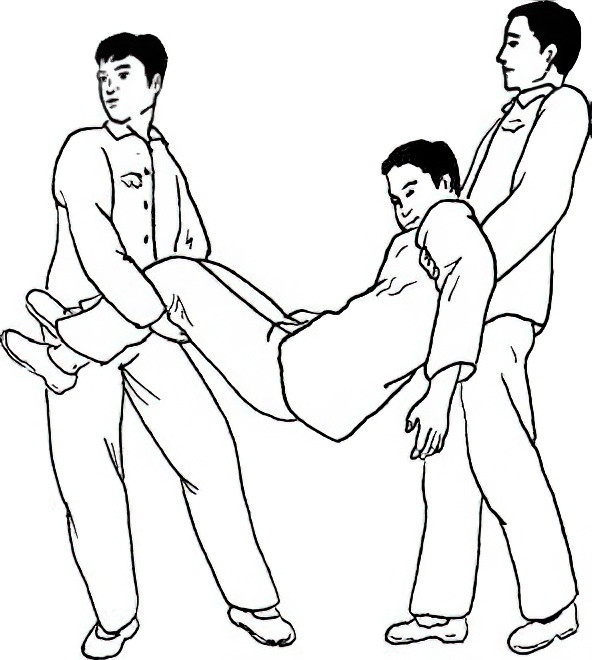
Figure 9 Incorrect transport method for spinal fracture patients
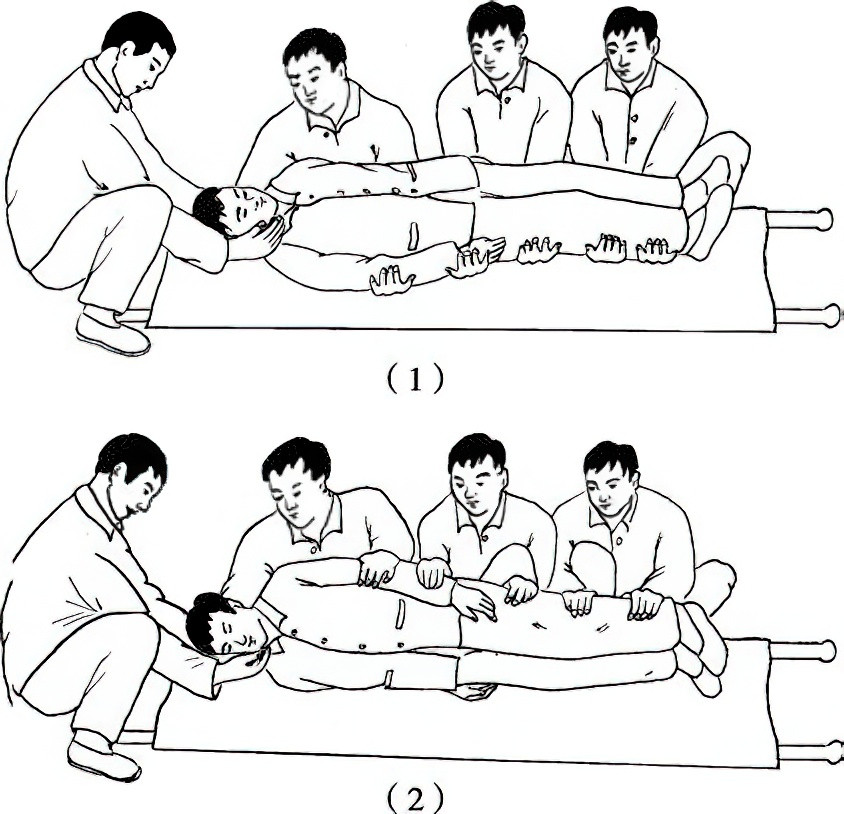
Figure 10 Correct transport methods for spinal fracture patients
1, Flat support method
2, Rolling method
Treatment
Cervical Spine Injuries
Upper Cervical Spine (Atlas and Axis) Injuries
Atlas Fractures of the Anterior and Posterior Arches
These are also known as Jefferson fractures. The fracture fragments displace outward without compressing the spinal cord, and no symptoms of spinal cord compression are observed. Treatment typically involves halo vest fixation for 12 weeks or cranial traction.
Atlantoaxial Dislocations
This type of injury occurs due to rupture of the transverse ligament, alar ligaments, and apex dens ligament, leading to dislocation between the odontoid process of the axis and the anterior arch of the atlas. This condition may compress the spinal cord and is considered an unstable injury. Treatment usually involves reduction under traction, followed by atlantoaxial fusion surgery.
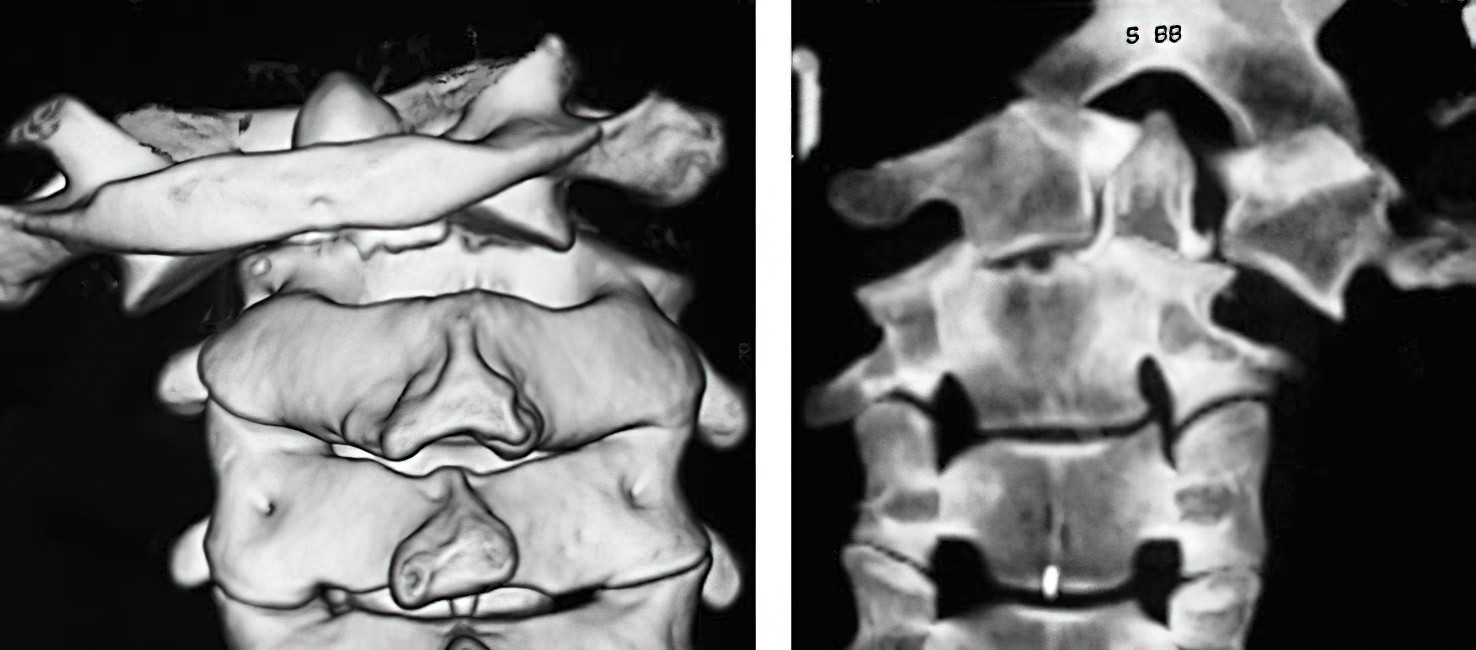
Figure 11 Atlantoaxial dislocation
Odontoid Fractures
Type I, Type III, and non-displaced Type II odontoid fractures are generally treated non-surgically with halo vest fixation for 6–8 weeks for Type I and non-displaced Type II fractures, and for 12 weeks for Type III fractures.
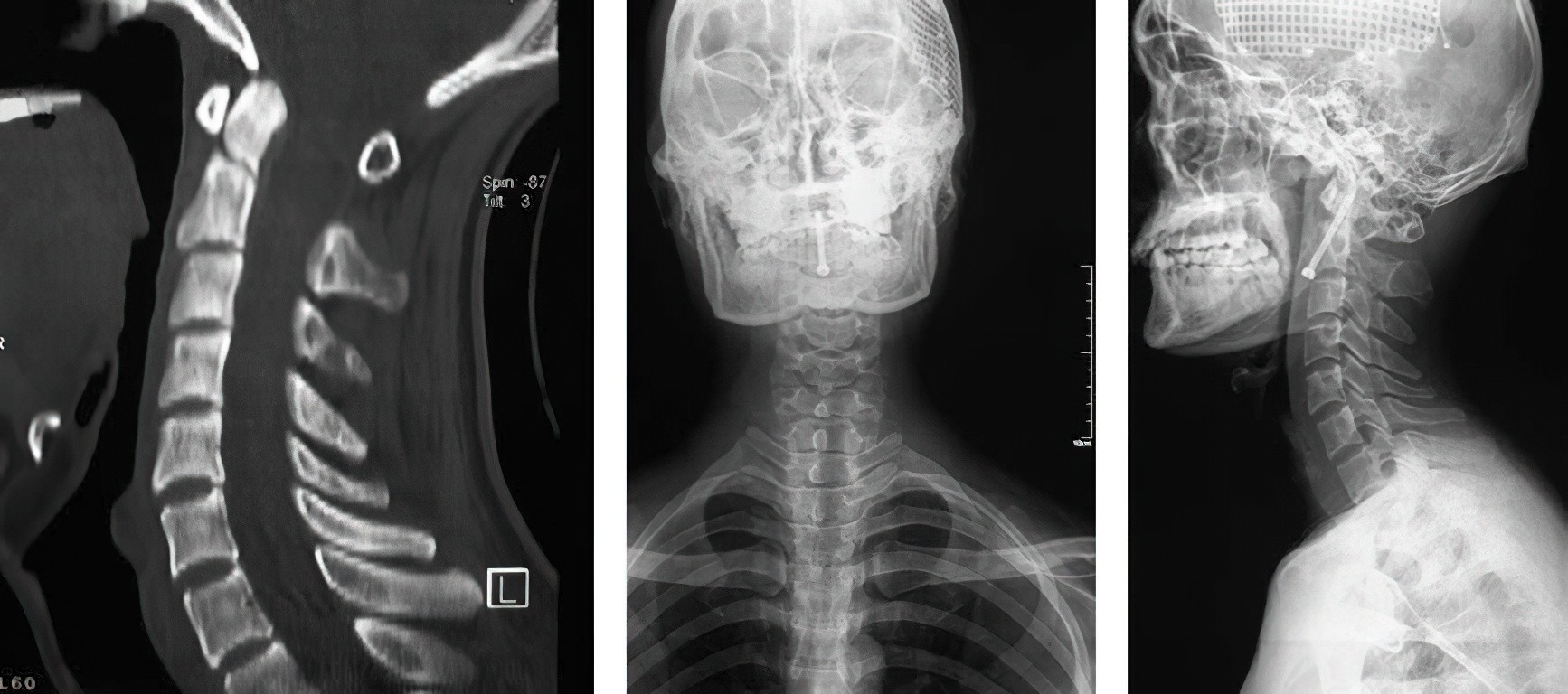
Figure 12 Internal fixation of odontoid fractures via anterior hollow screw
Displaced Type II fractures with a displacement greater than 4 mm usually have a low healing rate, and surgical treatment is often recommended. This can involve anterior fixation with 1–2 hollow screws or posterior C1–C2 transarticular screw fixation combined with bone grafting and fusion.
Fractures of the Axis Pedicles
Non-displaced fractures are treated with traction or halo vest fixation for 12 weeks. If anterior displacement of the vertebral body is present, it indicates traumatic spondylolisthesis of the axis, which may require cranial traction, bone grafting, and internal fixation for reduction and stabilization.
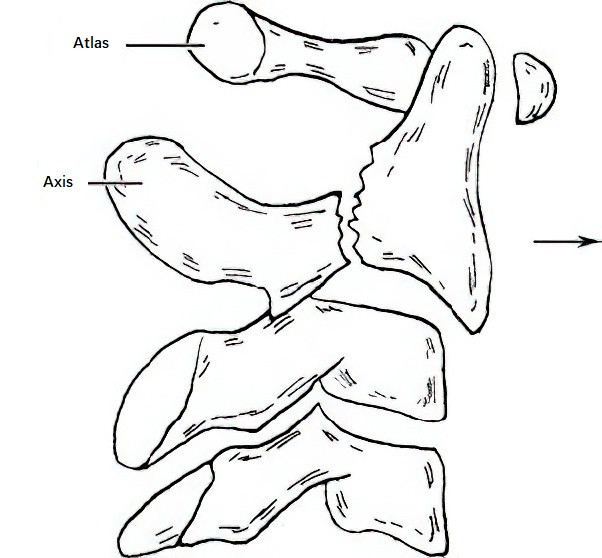
Figure 13 Axis pedicle fracture with traumatic spondylolisthesis
Lower Cervical Spine (C3–C7) Injuries
Compression Fractures
For fractures where the vertebral body height compression is less than one-third, head, neck, and thoracic supports are used for fixation for 8–12 weeks. Unstable fractures with more than one-third compression require subtotal corpectomy, bone grafting, and internal fixation.
Burst Fractures
These injuries often involve the spinal canal and are associated with spinal cord compression. Before treatment, the extent of spinal cord injury, spinal canal involvement, and posterior structural integrity should be evaluated. Management typically involves anterior surgery, including subtotal corpectomy, bone grafting, and internal fixation.
Fracture-Dislocations
If there is no intervertebral disc herniation, treatment may involve cranial traction reduction followed by anterior interbody fusion or posterior open reduction and fixation.
In cases of acute intervertebral disc herniation, anterior discectomy, bone grafting, and internal fixation are performed before conducting posterior open reduction and fixation.
Hyperextension Cervical Spine Injuries
Patients with cervical stenosis are more prone to spinal cord compression due to reduced canal volume during hyperextension. Treatment options include posterior laminoplasty to enlarge the canal size (single-door or double-door techniques) or laminectomy combined with decompression and bone grafting with internal fixation.
Thoracolumbar Spine Injuries
Historically, classifications of thoracolumbar spine fractures have focused predominantly on the description of fracture morphology, which provided limited guidance for clinical treatment and prognosis. To address this, Vaccaro et al. proposed the Thoracolumbar Injury Classification and Severity Score (TLICS). This system evaluates the injury mechanism, integrity of the posterior ligamentous complex, and neurological involvement to guide whether surgical treatment is necessary.
- A TLICS score of 5 or higher indicates the need for surgical treatment.
- A score of 3 or lower suggests non-surgical treatment.
- A score of 4 allows for either surgical or non-surgical treatment.
In cases without neurological symptoms or with radicular symptoms, posterior surgery is recommended regardless of whether the posterior ligamentous complex is intact.
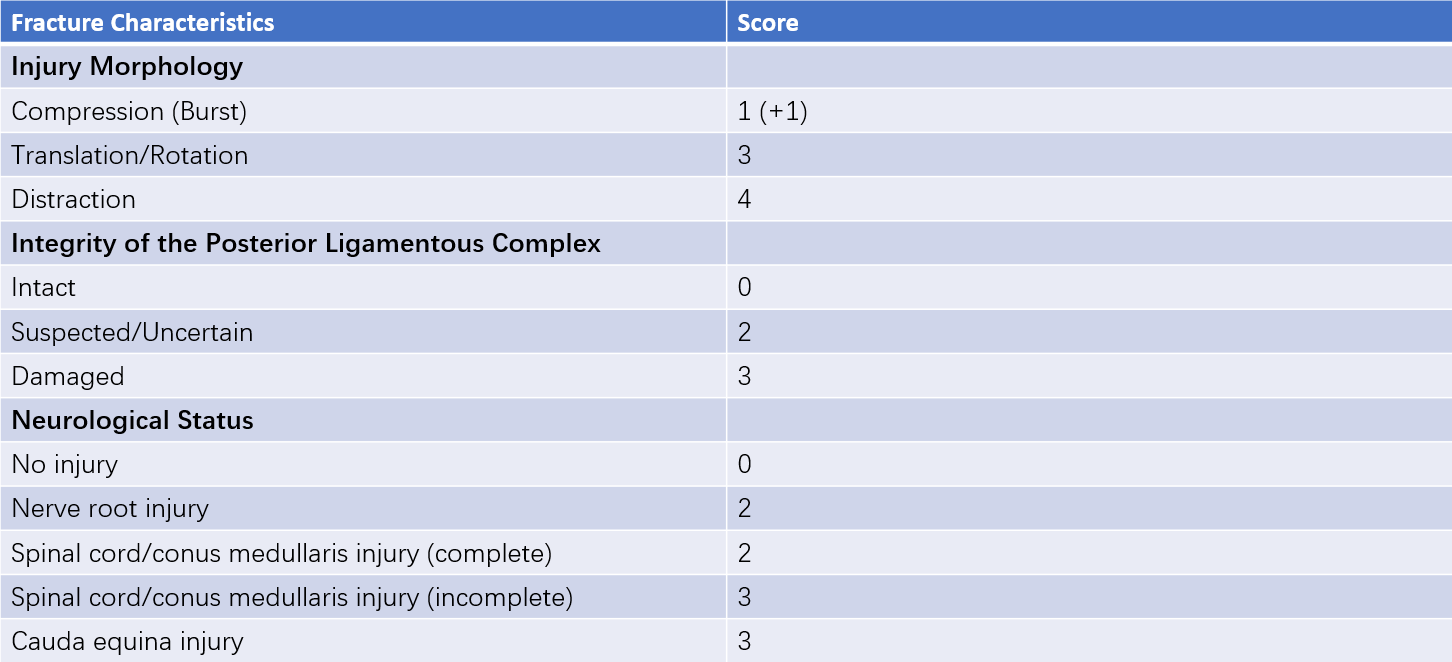
Table 1 TLICS scoring system
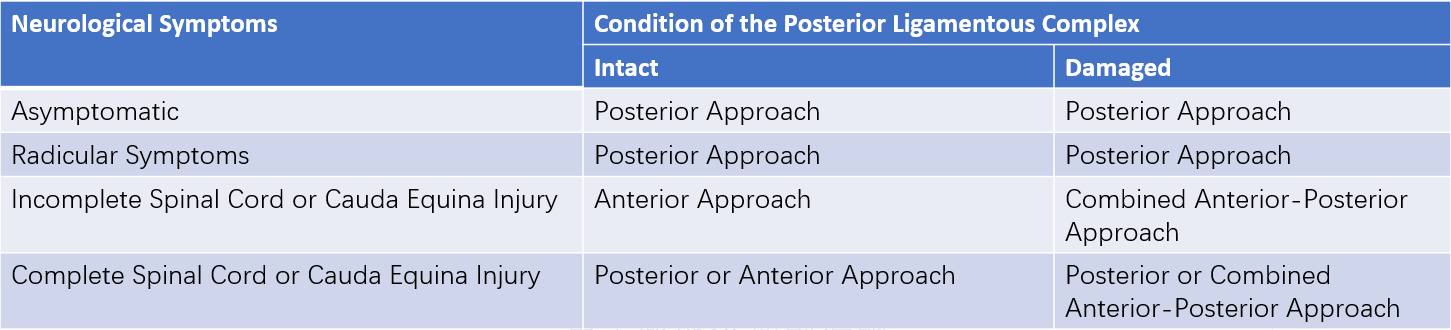
Table 2 Surgical approach selection based on TLICS scoring system
Incomplete spinal cord or cauda equina injuries with posterior ligamentous complex injury require a combined anterior-posterior approach. If the posterior ligamentous complex remains intact, an anterior approach is recommended.
Figure 14 Posterior reduction and pedicle screw fixation for lumbar burst fracture
Complete spinal cord or cauda equina injuries with posterior ligamentous complex injury may require either posterior surgery or a combined anterior-posterior approach. If the posterior ligamentous complex is intact, posterior or anterior surgery is appropriate.
For elderly patients with osteoporosis, minor trauma can result in osteoporotic compression fractures. In such cases, minimally invasive procedures such as percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP) are commonly used for clinical treatment.