Anatomical Overview
The gastrocnemius and soleus muscles in the posterior compartment of the lower leg converge distally to form the Achilles tendon, which inserts onto the posterior surface of the calcaneal tuberosity. The plantaris tendon descends medially alongside it. The primary function of the Achilles tendon is to enable plantar flexion of the ankle joint, maintain ankle balance, and support activities such as running, jumping, and walking.
Etiology and Classification
Achilles tendon rupture can be caused by direct trauma, such as a blow from a heavy object, resulting in contusion, partial, or complete rupture of the tendon—often accompanied by skin injury. Indirect trauma is more common and typically results from sudden, forceful muscle contraction, such as during improper takeoff or landing. In these cases, a sudden and powerful contraction of the triceps surae may tear the tendon.
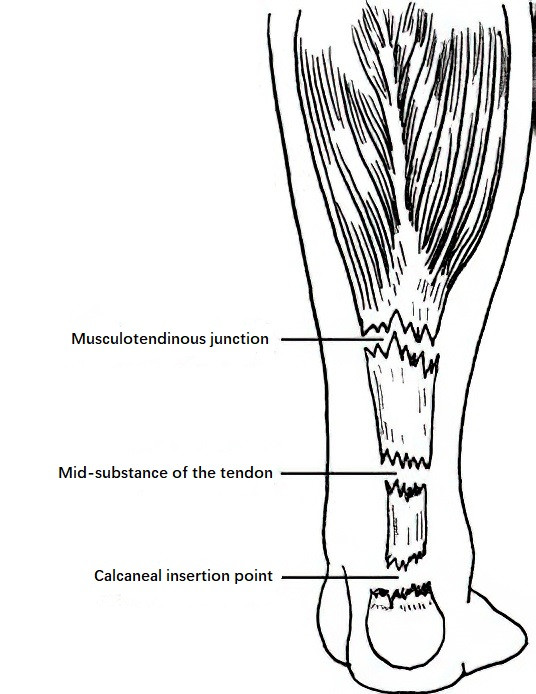
Figure 1 Common sites of achilles tendon rupture
Tendon injury may occur at the insertion point, the mid-portion, or the musculotendinous junction. These tears are often frayed and irregular in appearance. Injury can also be caused by sharp objects, such as glass or knives, producing relatively clean open wounds with less contamination.
Clinical Manifestations and Diagnosis
At the moment of injury, a snapping sound may be heard, followed by immediate heel pain, swelling, bruising, weakness in walking, and an inability to perform heel raises. On examination, tenderness and a palpable gap or soft defect may be noted at the rupture site. In cases of partial rupture, functional impairment may not be obvious, leading to misdiagnosis as a soft tissue injury. Ultrasound imaging can be used to localize and classify the tendon injury.
Treatment
Partial closed Achilles tendon ruptures, which are rare, may heal spontaneously with immobilization using a plaster cast for 4–6 weeks while the ankle is positioned in plantar flexion and the leg is relaxed. Functional rehabilitation is then recommended to aid recovery.
For complete ruptures, early surgical intervention is generally required. The tendon may be repaired through open or minimally invasive techniques. Postoperatively, the knee is flexed and the ankle is immobilized in plantar flexion using a plaster cast for 4–6 weeks, followed by progressive functional training.
For open Achilles tendon injuries, early debridement and tendon repair are essential. If direct skin closure produces excessive tension and risks skin necrosis with tendon exposure, skin flap transfer may be used to cover the tendon. Chronic complete ruptures of the Achilles tendon usually require surgical treatment.