Anatomical Overview
The ankle joint is composed of the distal ends of the tibia and fibula, along with the body of the talus. The medial malleolus is the protrusion at the medial distal end of the tibia, while the posterior margin forms the posterior malleolus. The lateral malleolus is the protrusion at the distal end of the fibula. The lateral malleolus is positioned slightly posterior to the medial malleolus and does not lie in the same coronal plane. Additionally, it is located 1–1.5 cm lower and 1 cm posterior compared to the distal end of the medial malleolus. Together, the medial malleolus, lateral malleolus, and the tibial plafond form the mortise, which encloses the body of the talus, creating the ankle joint. The anterior portion of the talus is wider than the posterior, providing greater congruency during dorsiflexion and stabilizing the ankle joint. In contrast, plantarflexion creates a larger gap between the talus and the mortise, increasing joint mobility but reducing stability. This anatomical feature accounts for the ankle joint’s predisposition to injuries during plantarflexion. The articular surface of the talar dome contacts two-thirds of the tibial plafond, making the ankle a primary weight-bearing joint. During walking, the joint bears forces approximately twice the body weight during mid-stance and up to five times the body weight during the late stance phase. This significant load contributes to the risk of injury and degenerative arthritis in the ankle joint. Under normal conditions, the neutral position of the ankle joint is defined as 0°, with the lateral edge of the foot perpendicular to the lower leg. The ankle has a range of motion of 20°–30° in dorsiflexion and 45°–50° in plantarflexion. Inversion and eversion movements primarily occur at both the ankle joint and the subtalar joint, with ranges of approximately 30° for inversion and 30°–35° for eversion, where the subtalar joint plays a larger role.
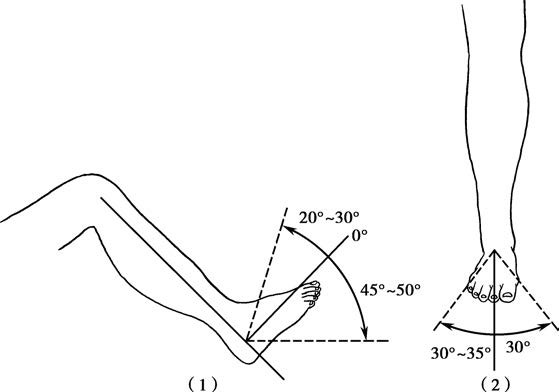
Figure 1 Range of motion of the ankle joint
(1) Dorsiflexion and plantarflexion range of motion
(2) Inversion and eversion range of motion
Etiology and Classification
Ankle fractures often result from indirect forces, most commonly involving sprains during plantarflexion. They account for 7.6% of adult fractures. The fracture type depends on the magnitude, direction of force, and the position of the foot and ankle at the time of injury. Direct trauma can also lead to more complex fracture patterns. Various classification systems have been developed for ankle fractures, with the Lauge-Hansen and Danis-Weber systems being commonly used.
Lauge-Hansen Classification
This system emphasizes the pathological morphology of fractures that occur under different injury positions, injury types, and force magnitudes, aiming to explain the mechanisms behind different fracture patterns.
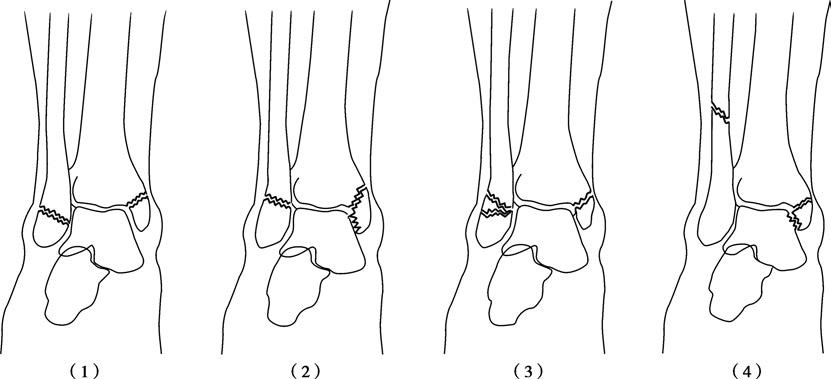
Figure 2 Classification of ankle fractures (Lauge-Hansen method)
Supination-Adduction (SA)
"Supination" refers to the position of the foot at the time of injury, similar to the supination of the forearm, with the plantar surface facing inward and forward. "Adduction" represents the direction of force, which causes the talus to exert inversion stress within the mortise. Type I involves avulsion of the lateral malleolus or a ligamentous tear due to tension. Type II involves a medial malleolar fracture, with the fracture line running obliquely from the medial upper corner of the mortise.
Supination-External Rotation (SER)
This is the most common type of injury. "Supination" has the same meaning as above. "External rotation" refers to the direction of force causing the talus to externally rotate in the mortise pivoting around the posteromedial axis. Type I starts with the rupture of the anterior inferior tibiofibular ligament. Type II involves a fibular fracture at the syndesmosis level, with the fracture line extending from the anterior-inferior direction to the posterior-superior direction. Type III includes rupture of the posterior inferior tibiofibular ligament or posterior malleolar fracture. Type IV includes a deltoid ligament rupture or a medial malleolar avulsion fracture.
Pronation-Abduction (PA)
During this type of injury, the foot is in a pronated position (with the plantar surface facing outward and backward), and the force acts to abduct the ankle laterally. Type I starts with tension-induced damage to the medial side, causing a medial malleolar fracture or rupture of the deltoid ligament. Type II involves rupture of the anterior and posterior tibiofibular ligaments or fractures at the anterior tibial tubercle or posterior malleolus. Type III involves an oblique or comminuted fracture of the lateral malleolus at the syndesmosis level or slightly above.
Pronation-External Rotation (PER)
"Pronation" retains the same definition as above. "External rotation" describes force applied to the talus, causing it to externally rotate with its posterolateral aspect serving as an axis within the mortise. Type I involves medial tensile damage such as a medial malleolar fracture or rupture of the deltoid ligament. Type II involves rupture of the anterior tibiofibular ligament. Type III involves a spiral or oblique fracture of the lateral malleolus occurring 6–10 cm above the syndesmosis level. Type IV includes rupture of the posterior tibiofibular ligament or posterior malleolar fracture.
Danis-Weber Classification
This system categorizes fractures of the lateral malleolus based on their height relative to the tibiofibular syndesmosis, serving as a guide for surgical management.
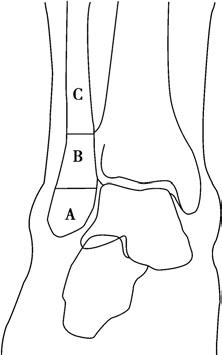
Figure 3 Danis-Weber classification of ankle fractures
Classification based on the level of fibular fractures relative to the height of the ankle joint.
Type A: The fibular fracture line lies below the ankle joint plane.
Type B: The fibular fracture line is at the level of the ankle joint.
Type C: The fibular fracture line lies above the level of the ankle joint.
Type A
Lateral malleolar fractures below the syndesmosis level, corresponding to the Supination-Adduction type in the Lauge-Hansen classification.
Type B
Lateral malleolar fractures at the level of the syndesmosis, corresponding to the Lauge-Hansen Supination-External Rotation and Pronation-Abduction types.
Type C
Lateral malleolar fractures above the syndesmosis, corresponding to the Lauge-Hansen Pronation-External Rotation type.
Clinical Presentation and Diagnosis
Ankle injuries commonly present with significant swelling, bruising, and deformities such as inversion or eversion. Movement is often restricted, and local tenderness is noticeable. Bone crepitus may be palpated. Anteroposterior and lateral X-rays of the ankle joint are useful for identifying the fracture location, displacement, and type. In Type III fractures, the entire length of the fibula should be examined. If tenderness is noted near the fibular head, additional X-rays of the proximal fibula may help confirm the presence of fractures.
Treatment
The ankle joint is complex in structure, and the mechanisms of injury and fracture types are diverse. The primary treatment principle involves restoring the structure and stability of the ankle joint based on a thorough understanding of the injury characteristics. Treatment plans are selected flexibly, usually starting with closed reduction and external fixation. If satisfactory reduction and fixation cannot be achieved or if treatment fails, minimally invasive or open reduction with internal fixation is employed.
Without detailed analysis of factors such as the injury mechanism, direction of displacement, and ankle joint stability, hasty treatment can exacerbate fracture displacement, cause new injuries, and complicate subsequent treatment and functional recovery. For non-displaced fractures or isolated medial or lateral malleolar fractures without tibiofibular syndesmosis separation, a plaster cast is applied in a neutral ankle position or inversion (for medial malleolar fractures) / eversion (for lateral malleolar fractures) position for 6–8 weeks. During the immobilization period, adjacent joint function exercises aim to prevent deep vein thrombosis and muscle atrophy.
For displaced solitary medial or lateral malleolar fractures, manual reduction is often unsuccessful due to ligament laxity, and even if achieved, maintaining ligament tension is difficult. Minimally invasive or open reduction with internal fixation is typically required. For injuries involving tibiofibular syndesmosis separation, reduction and fixation of the malleolar fractures are necessary to restore syndesmotic alignment. To prevent postoperative instability, syndesmotic fixation is achieved using screws, high-strength sutures, or elastic fixation devices. Screw fixation provides rigid stabilization and should typically be removed 10–12 weeks post-surgery before partial weight-bearing to avoid screw loosening or breakage.
Type I fractures, involving bimalleolar fractures, generally require minimally invasive or open reduction to restore ligament tension. Internal fixation using cancellous screws or bone plates with screws is employed.
Type II fractures, or trimalleolar fractures, necessitate cancellous screw fixation for medial malleolar fractures. Lateral malleolar fractures often require fixation using bone plates. When posterior malleolar fractures affect 25%–33% of the articular surface, internal fixation is also indicated.
For Type III fractures, in addition to internal fixation for medial, lateral malleolar, or fibular fractures, fixation of the fibula plays a crucial role in ensuring distal tibiofibular stability.
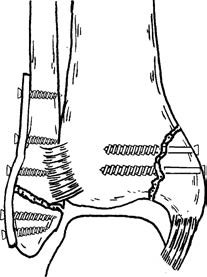
Figure 4 Open reduction and internal fixation for bimalleolar fractures
In all three fracture types, soft tissue injuries such as ligament or joint capsule ruptures should be repaired simultaneously. Vertical compression fractures often require open reduction and internal fixation. The compressed and collapsed area is reduced, and residual bone loss is filled with autologous bone or artificial bone grafts.