Anatomical Overview
The tibia is a key weight-bearing bone, and its anterior crest serves as an important landmark for manual fracture reduction. The cross-section of the upper and middle third of the tibial shaft is triangular, whereas the lower part is quadrangular, making the junction of these regions more susceptible to fractures. The tibia lies subcutaneously, and fractured bone ends may easily pierce the skin, resulting in open fractures.
The articular surfaces at the proximal and distal ends of the tibia are parallel; if this alignment is disrupted by a fracture, joint loading mechanics can be altered, increasing the risk of post-traumatic arthritis. The proximal and distal ends of the fibula form the superior and inferior tibiofibular joints with the tibia. These are amphiarthroses, with the fibula contributing no independent movement, but bearing about one-sixth of the body’s weight.
An interosseous membrane connects the tibia and fibula, and forces acting on the ankle joint are transmitted not only along the tibial shaft but also via the membrane to the fibula. After branching from the popliteal artery, the anterior tibial artery passes downward through the tendinous arch of the soleus muscle, a point where the vessel is relatively fixed. Fractures in the upper third of the tibia may damage this artery, causing significant circulatory impairment or even ischemic necrosis of the lower limb.
The leg contains four fascial compartments formed by the fascial structures in conjunction with the tibia, fibula, and interosseous membrane. Fracture-related bleeding from the medullary cavity or from muscle and vascular injury can lead to compartment syndrome, which may result in muscle ischemia and necrosis, subsequent fibrosis, and long-term functional impairment.
The nutrient artery enters the tibial shaft at the junction of the upper and middle thirds. Fractures in the middle to lower thirds may damage this artery, greatly reducing blood supply to the distal tibia. Furthermore, the distal third lacks muscular attachments and receives limited blood flow from the distal tibial vessels, contributing to slow healing and increased risk of delayed union or nonunion.
The common peroneal nerve runs obliquely downward and laterally from the posterior-lateral popliteal fossa, crossing the fibular neck before entering the lateral and anterior muscle groups of the lower leg. Displaced fractures at the fibular neck may injure the common peroneal nerve.
Etiology and Classification
Because the tibia and fibula are located superficially, they are easily injured by direct trauma. Diaphyseal fractures of the tibia and fibula account for approximately 4% of all fractures. The fracture pattern varies with the mechanism of injury:
- Direct trauma may produce transverse, short oblique, or comminuted fractures.
- Twisting forces may cause spiral or oblique fractures of both bones.
In double fractures, the fibular fracture line is typically located higher than that of the tibia.
In 89% of spiral fractures in the distal third of the tibia, a concomitant posterior malleolar fracture occurs. This is often missed and requires careful evaluation.
Diaphyseal fractures of the tibia and fibula can be classified into three types:
- Combined fractures of both the tibial and fibular shafts;
- Isolated tibial shaft fractures;
- Isolated fibular shaft fractures.
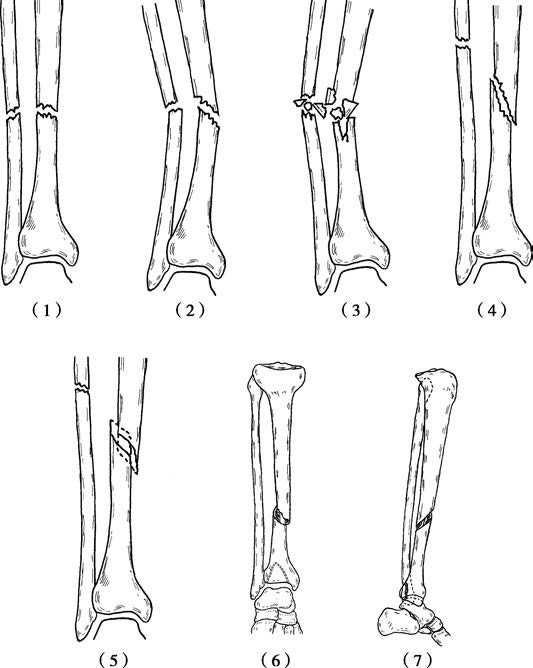
Figure 1 Types of tibiofibular fractures
(1) Transverse fracture
(2) Short oblique fracture
(3) Comminuted fracture
(4) Long oblique fracture
(5) Spiral fracture
(6) Spiral fracture of the distal third of the tibia with posterior malleolar fracture (anteroposterior view)
(7) Spiral fracture of the distal third of the tibia with posterior malleolar fracture (lateral view)
Combined fractures of both bones are most common and usually result from high-energy trauma, involving severe bone and soft tissue injury, with a higher risk of complications and treatment challenges. Isolated fibular fractures are uncommon and often result from direct trauma to the lateral leg. Isolated tibial shaft fractures are also rare, usually caused by low-energy direct trauma. Due to the supportive role of the fibula, displacement is typically minimal.
Treatment
The primary goals in treating tibiofibular diaphyseal fractures are to correct angular and rotational deformities, restore the parallel relationship of the proximal and distal tibial articular surfaces, and maintain limb length.
For non-displaced fractures, plaster cast immobilization is appropriate.
Displaced transverse or short oblique fractures may be managed with manual reduction followed by casting.
During immobilization, attention should be paid to cast tightness, and regular radiographic evaluation should be performed. Any signs of displacement warrant timely adjustment or re-casting. Partial weight-bearing with crutches is usually permitted after 10 to 12 weeks.
Unstable combined tibia and fibula fractures often require minimally invasive or open reduction and internal fixation using plates and screws or intramedullary nails. Partial weight-bearing with crutches is generally allowed 4 to 6 weeks postoperatively.
For open fractures of both bones, thorough debridement is essential. Fixation may be achieved with intramedullary nails or an external fixator, followed by local skin or musculocutaneous flap coverage to prevent exposure of implants or bone tissue.
In isolated tibial shaft fractures, displacement is generally minimal due to fibular support. Cast immobilization for 10 to 12 weeks is usually sufficient before initiating ambulation.
In isolated fibular shaft fractures without involvement of the superior or inferior tibiofibular joints, no special treatment is typically needed. A cast may be applied for 3 to 4 weeks to reduce pain.