Anatomical Overview
The upper end of the tibia interacts with the lower end of the femur to form the knee joint. The contact surface of the tibia with the femur is known as the tibial plateau, which includes two slightly concave surfaces. The medial and lateral menisci enhance these concave surfaces, allowing them to align closely with the corresponding surface of the femoral condyles, thereby improving stability of the knee joint. The tibial plateau serves as a crucial load-bearing structure of the knee, and fractures can lead to uneven stress distribution between the medial and lateral plateaus, potentially resulting in osteoarthritis over time. The medial and lateral collateral ligaments attach to the respective sides of the tibial plateau. Among tibial plateau fractures, 52.9% are accompanied by meniscal injuries, and 22.5% are associated with cruciate ligament injuries.
Etiology and Classification
Tibial plateau fractures are commonly caused by forces of varus, valgus stress, axial compression, or a combination of varus/valgus stress with axial compression. These fractures account for 1.7% of all fractures in adults. The injury mechanism of tibial plateau fractures is complex, with diverse clinical presentations and multiple classification systems. The Schatzker classification is currently the most widely used system, dividing tibial plateau fractures into six types:
- Type I: Lateral plateau split fracture without articular surface depression. This type often occurs in younger patients. Lateral meniscal tears frequently accompany displaced fractures, which may cause peripheral displacement or meniscal entrapment within the fracture gap. Type I accounts for 15.0% of tibial plateau fractures.
- Type II: Lateral plateau split fracture with articular surface depression, commonly seen in patients over 40 years of age. This type accounts for 23.2% of tibial plateau fractures.
- Type III: Pure compression fracture of the lateral plateau. The compressed area is often located at the central region of the articular surface. Depending on the size and degree of compression, as well as the condition of the lateral meniscus, this injury can present as either a stable or unstable fracture. Type III accounts for 14.5% of tibial plateau fractures.
- Type IV: Medial plateau fracture, typically caused by moderate-to-high energy trauma. It is often accompanied by knee dislocation and vascular injury, requiring careful examination. Type IV accounts for 14.5% of tibial plateau fractures.
- Type V: Bicondylar plateau fracture caused by high-energy trauma, frequently associated with vascular and neurological injuries. Type V accounts for 12.0% of tibial plateau fractures.
- Type VI: Bicondylar plateau fracture with separation between the diaphysis and metaphysis, resulting from high-energy trauma. X-rays typically show comminuted, burst-like fractures, often accompanied by severe soft tissue damage, compartment syndrome, and significant neurovascular injury. Type VI accounts for 20.8% of tibial plateau fractures.
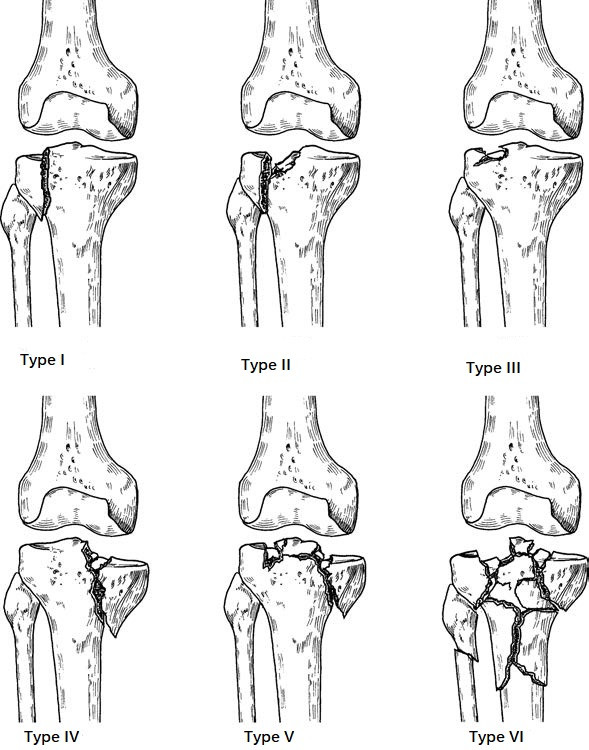
Figure 1 Schatzker classification for tibial plateau fractures
Although Schatzker classification is widely applied in clinical practice, it has limitations in encompassing all types of tibial plateau fractures. Other systems, such as the three-column classification and comprehensive classification, have gained popularity in recent years as tools to guide treatment strategies. Each classification method has its strengths and weaknesses, and none is universally considered flawless.
Clinical Manifestations
Tibial plateau fractures are characterized by symptoms such as knee pain, swelling, and inability to bear weight on the affected leg. Both active and passive knee joint motion are limited, with local tenderness noted in the proximal tibia and knee joint. Attention should be given to the condition of overlying soft tissue at the fracture site, as well as the neurological and vascular status. Prompt detection of potential injury to the popliteal artery is crucial. In cases of high-energy tibial plateau fractures, evaluation should focus on signs such as resting pain in the affected limb, severe pain induced by passive stretching of associated muscles, tightness of the leg (suggesting compartment syndrome), and diminished sensation in the foot.
Imaging Studies
Standard anteroposterior and lateral X-rays suffice for diagnosing fractures. CT can provide detailed insights into the displacement of fracture fragments and the morphology of articular surface depression. MRI offers a clear depiction of associated injuries to structures such as the menisci, ligaments, articular cartilage, and surrounding soft tissues, and can also identify bone bruising to assess the severity of injury. High-energy tibial plateau fractures (e.g., Schatzker Type IV, V, and VI) or knee dislocations may result in vascular damage, warranting angiographic evaluation in cases of suspected vascular injury or unexplained compartment syndrome.
Treatment
The goals of tibial plateau fracture treatment include restoring the smoothness of the articular surface, preserving the plateau width, maintaining ligament integrity, and ensuring sufficient range of knee motion. Non-displaced tibial plateau fractures can be managed with plaster immobilization for 4–6 weeks, followed by functional exercises. Displaced tibial plateau fractures are classified as unstable intra-articular fractures and require anatomical reduction and strong fixation. Bone defects at the fracture site call for bone grafting. Early rehabilitation principles include early exercises with delayed weight-bearing to promote recovery. Gradual activity may begin at 6–8 weeks, with full weight-bearing permitted only after fracture healing. Conventional open reduction and internal fixation are associated with significant trauma and complications, prompting a trend toward minimally invasive techniques.
Recent approaches advocate for double reverse traction as a minimally invasive option for tibial plateau fractures. Preoperative planning based on CT imaging helps determine positions for elevating depressed bone fragments. Double reverse traction devices facilitate sustained, controlled traction during surgery, enabling indirect reduction of lateral displaced fracture fragments via soft tissue compression and rapid correction of lower limb alignment and joint dislocation. Techniques such as bone elevation using reduction rods, compression using bolts, and minimal invasive fixation methods are combined to stabilize fracture fragments and restore function effectively.
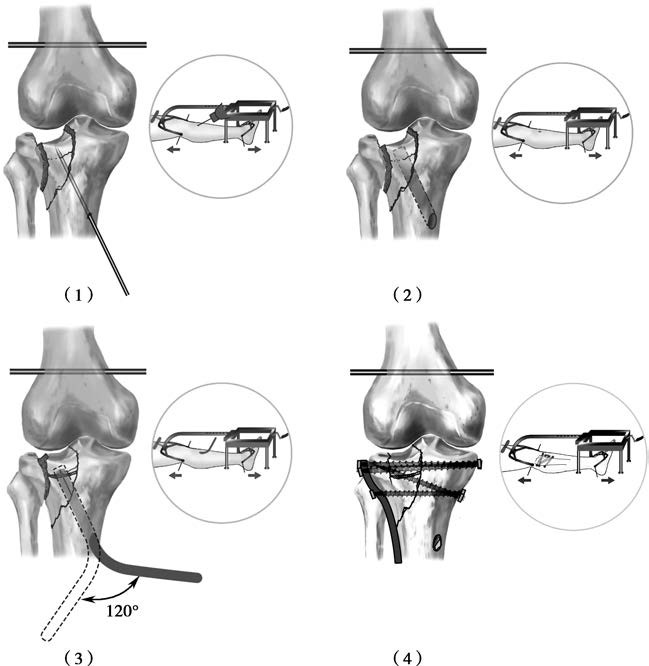
Figure 2 Double reverse traction treatment for tibial plateau fractures
(1) Placement of guide pin into depressed fracture fragment
(2) Expansion of pathway along the guide pin
(3) Elevation of depressed fracture using reduction rod
(4) Placement of anatomical fixation plate and compression bolts via minimally invasive techniques