Anatomical Overview
Femoral shaft fractures involve fractures of the bone segment between the subtrochanteric region and the supracondylar area. The femoral shaft is the thickest, longest, and most load-bearing tubular bone in the human body. Its bending strength is comparable to cast iron, yet it exhibits superior elasticity. Due to its anatomical and biomechanical properties, femoral shaft fractures typically result from high-energy trauma and require prolonged healing and remodeling periods. These fractures account for approximately 2.2% of adult fractures. The femoral shaft has a slight anterior and lateral curvature. Posteriorly, it features the linea aspera, a ridge serving as the attachment site for muscles involved in knee flexion and extension. The forces causing femoral shaft fractures often damage surrounding muscles, fascia, and soft tissues. Subsequent hematoma organization, fibrosis, adhesions, and immobilization further impair muscle function, leading to restricted knee mobility.
Etiology and Classification
Direct Trauma
Injuries such as heavy object impacts, vehicular crushing, or ballistic wounds typically result in transverse or comminuted fractures with extensive soft tissue damage.
Indirect Trauma
Falls from heights or torsional forces (e.g., machinery accidents) often produce oblique or spiral fractures with milder soft tissue involvement.
Femoral shaft fractures can be classified into fractures of the proximal third, middle third, and distal third of the shaft. Each location exhibits characteristic displacement patterns due to the pull of attached muscles at their points of origin and insertion.
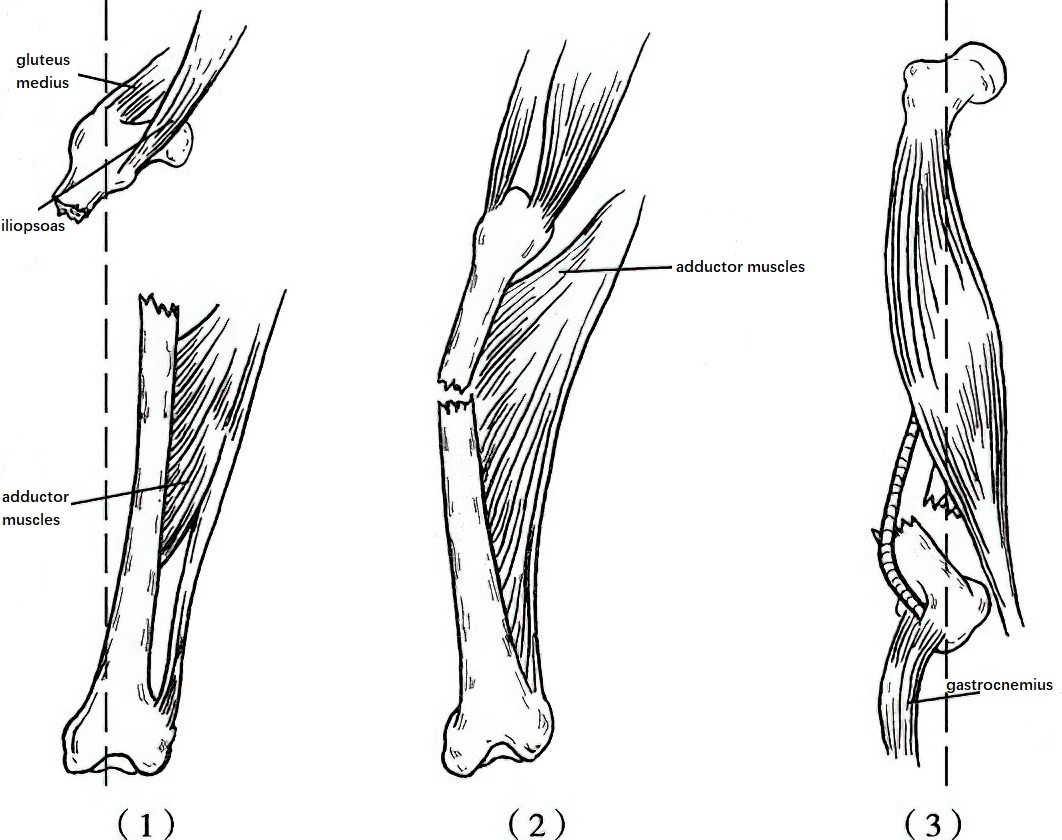
Figure 1 Displacement directions of femoral shaft fractures at different locations
(1) Proximal third of the femoral shaft
(2) Middle third of the femoral shaft
(3) Distal third of the femoral shaft
In fractures of the proximal third, the proximal fragment displaces anteriorly, laterally, and rotates externally due to the pull of the iliopsoas muscle, gluteus medius, gluteus minimus, and external rotator muscles. The distal fragment displaces proximally and posteriorly under the combined action of the quadriceps, tensor fasciae latae, and adductor muscles.
In fractures of the middle third of the shaft, the fracture ends form an angular deformity outward due to the traction exerted by the adductor muscle group.
In fractures of the distal third, the distal fragment displaces posteriorly because of the pull of the gastrocnemius muscle and the effect of limb gravity. Additionally, under the combined traction forces of the vastus lateralis, vastus medialis, and vastus intermedius muscles, the proximal fragment displaces anteriorly, resulting in overlapping of the fracture ends and creating shortening deformities.
The direction of displacement of femoral shaft fractures is influenced not only by muscle traction but also by factors such as the direction and magnitude of the traumatic force, the position of the limb during injury, and the conditions of emergency transport.
Clinical Manifestations and Diagnosis
A clinical diagnosis can be made based on the distinctive features of the fracture observed after injury. Anteroposterior and lateral X-ray imaging can clearly identify the exact location, type, and displacement of the fracture. In cases of fractures in the distal one-third of the femoral shaft, posterior displacement of the distal fracture fragment may occur, which has the potential to cause injury to the popliteal artery, popliteal vein, tibial nerve, and common peroneal nerve. It is therefore necessary to carefully examine the blood circulation, as well as the sensory and motor functions, of the distal limb. Single femoral shaft fractures, due to significant blood loss, may present with pre-shock clinical symptoms. If multiple fractures or bilateral femoral shaft fractures are present, the likelihood of shock increases considerably. A proper assessment of the patient's overall condition is required.
Treatment
Non-Surgical Treatment
For children under the age of three, vertical suspension skin traction is used (Figure 2). During the traction process, regular measurement of limb length and bedside X-rays are performed to ensure the traction force is sufficient. Excessive traction, leading to separation of fracture ends, could result in delayed union or nonunion of the fracture.
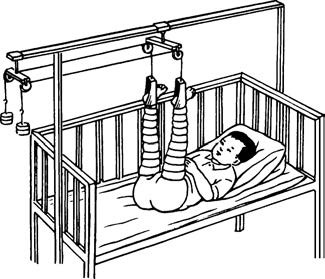
Figure 2 Vertical suspension skin traction in children
In recent years, surgical internal fixation has been the preferred treatment method for femoral shaft fractures in adults and children over three years old. For patients with contraindications to surgery, continuous traction for 8 to 10 weeks is an option. During the period of bedridden management, muscle contraction exercises are emphasized to prevent muscle atrophy, joint adhesions, and deep vein thrombosis. Gradual mobilization is introduced after bedside X-rays confirm fracture union.
Surgical Treatment
Locked intramedullary nailing is commonly used for adult femoral shaft fractures. Elastic intramedullary nails are the preferred method for internal fixation in children with femoral shaft fractures. Severe open fractures are treated with external fixation devices.
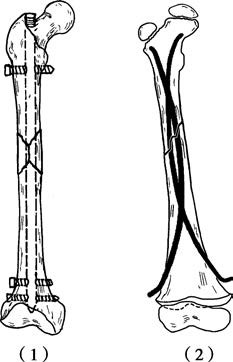
Figure 3 Internal fixation methods for femoral shaft fractures
(1) Locked Intramedullary Nailing
(2) Elastic Nail Fixation