Anatomical Overview
The proximal femur features the greater trochanter laterally and the lesser trochanter medially. Both the greater trochanter, lesser trochanter, and the intertrochanteric region consist of cancellous bone. The intertrochanteric region, located at the junction of the femoral shaft and neck, is subjected to the highest shear stress within the femur. Due to the unique biomechanical force distribution, a dense vertical bony plate—termed the femoral calcar (calcar femorale)—forms posteromedially at the femoral neck-shaft junction. The integrity of the femoral calcar critically determines the stability of intertrochanteric fractures.
Etiology and Classification
Similar to femoral neck fractures, intertrochanteric fractures commonly occur in middle-aged and elderly individuals with osteoporosis, accounting for 3.4% of fractures in adults. Intertrochanteric fractures are often caused by indirect trauma, such as falls that involve body rotation, which occur when landing in an excessive abduction or adduction position. Direct trauma, such as falling onto the side with direct impact on the greater trochanter, can also lead to intertrochanteric fractures. The intertrochanteric region is also a common site of cystic bone lesions, making pathological fractures possible. Distinguishing between these two conditions is necessary.
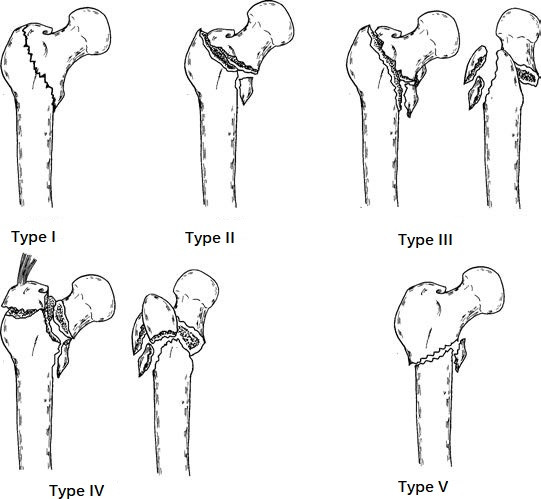
Figure 1 Tronzo-Evans classification of intertrochanteric fractures
There are several classification methods for intertrochanteric fractures. Based on the Tronzo-Evans classification system, intertrochanteric fractures can be categorized into five types:
- Type I: Intertrochanteric fracture with no displacement, considered a stable fracture and accounting for 11.1% of intertrochanteric fractures.
- Type II: Fracture with minor involvement of the lesser trochanter and a stable reduction, classified as a stable fracture and making up 17.4% of intertrochanteric fractures.
- Type III: Comminuted fracture of the lesser trochanter, where a stable reduction cannot be achieved, considered an unstable fracture and comprising 45.1% of intertrochanteric fractures.
- Type IV: Unstable fracture involving both Type III characteristics and an additional fracture of the greater trochanter, accounting for 20.1% of intertrochanteric fractures.
- Type V: Reverse intertrochanteric fracture with displacement tendency due to pull from the adductor muscles, classified as an unstable fracture and representing 6.3% of intertrochanteric fractures.
Clinical Manifestations and Diagnosis
Following injury, symptoms include pain in the trochanteric region, swelling, bruising, and inability to move the lower extremity. Tenderness is observed in the intertrochanteric region, along with a pronounced external rotation deformity of the lower limb, which may reach up to 90°. Axial percussion pain is present, and measurement often reveals shortening of the lower limb. X-ray imaging is employed to confirm the fracture type and evaluate the degree of displacement.
Treatment
Non-Surgical Treatment
For patients with contraindications to surgery, tibial tuberosity traction or supracondylar femoral traction in an abduction position is performed. After 10 to 12 weeks, gradual mobilization with crutches may begin. Intertrochanteric fractures primarily affect elderly individuals and are associated with osteoporosis. Non-surgical treatment requires prolonged bedrest, which is associated with higher complication rates and increased mortality. In recent years, early surgical intervention has been advocated.
Surgical Treatment
The goal of surgical treatment is to achieve anatomical reduction as far as possible, restore the continuity of the calcar femorale, correct coxa vara deformity, provide strong internal fixation, enable early mobilization, and prevent complications. Various methods of internal fixation are available, including Gamma nails, dynamic hip screws (DHS), proximal femoral anti-rotation nails (PFNA), and proximal femoral bionic nails (PFBN).
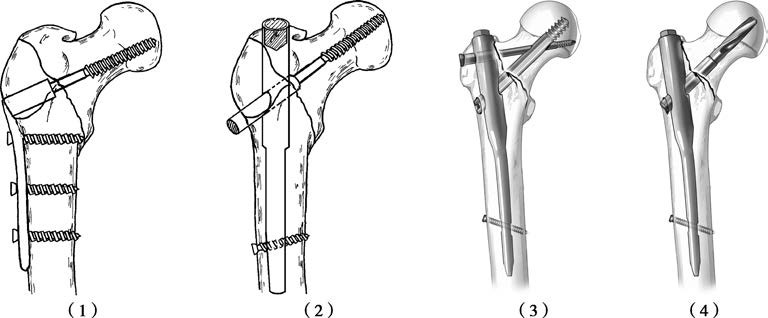
Figure 2 Internal fixation methods for intertrochanteric fractures
(1) Fixation with Dynamic Hip Screw (DHS)
(2) Fixation with Gamma Nail
(3) Fixation with Proximal Femoral Anti-Rotation Nail (PFNA)
(4) Fixation with Proximal Femoral Bionic Nail (PFBN)