Anatomical Overview
The hip joint, formed by the femoral head, femoral neck, and acetabulum, serves as a critical connection and weight-bearing structure between the trunk and lower limbs. The neck-shaft angle—formed between the longitudinal axis of the femoral neck and the femoral shaft—ranges from 110° to 140°, averaging 127°. This angle differs between children and adults, with children exhibiting a larger neck-shaft angle. During weight transmission, forces are not distributed along the central axis of the femoral neck but instead follow a path along the lesser trochanter and the medial border of the femoral neck. An increased neck-shaft angle results in coxa valga, while a decreased angle leads to coxa vara. Alterations in this angle disrupt force distribution, predisposing individuals to fractures, articular cartilage degeneration, and traumatic arthritis. The femoral neck anteversion angle, defined as the angle between the femoral neck axis and the coronal plane of the body, is slightly larger in children than in adults. This angle must be carefully considered during femoral neck fracture reduction and artificial joint replacement.
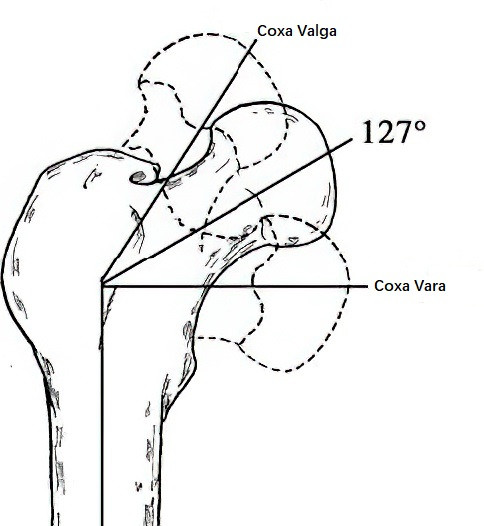
Figure 1 Cervicodiaphyseal angle of the femur
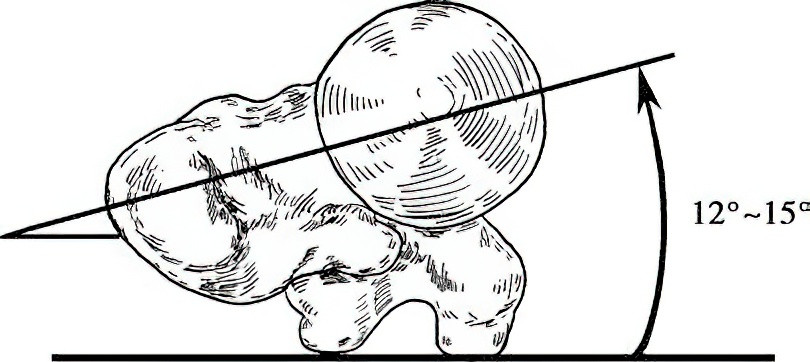
Figure 2 Femoral neck anteversion angle
The hip joint capsule is expansive, encasing the acetabulum, femoral head, and femoral neck from all directions. Notably, the portion of the femoral neck within the capsule lacks periosteum. The posterior, lateral, and inferior aspects of the joint remain unencapsulated. Ligaments such as the iliofemoral ligament (anterior-superior) and the ischiofemoral ligament (posterior-superior-medial) stabilize the joint.
In adults, the blood supply to the femoral head originates from three primary sources:
- The foveal artery within the ligamentum teres, which nourishes the fovea of the femoral head.
- The ascending branches of the femoral nutrient artery, extending along the femoral neck into the femoral head.
- Branches of the medial and lateral femoral circumflex arteries, which are vital for femoral head and neck perfusion.
The medial femoral circumflex artery, arising from the deep femoral artery, divides into the lateral epiphyseal artery, superior metaphyseal artery, and inferior metaphyseal artery at the synovial reflection of the femoral neck base. The lateral epiphyseal artery supplies 2/3 to 4/5 of the femoral head, serving as its primary blood source. Injury to the medial femoral circumflex artery is a leading cause of femoral head avascular necrosis.
The lateral femoral circumflex artery, also branching from the deep femoral artery, contributes partially to femoral head vascularization. Branches of the medial and lateral femoral circumflex arteries anastomose at the femoral neck base, forming an arterial ring that further distributes nutrient vessels to the femoral neck.
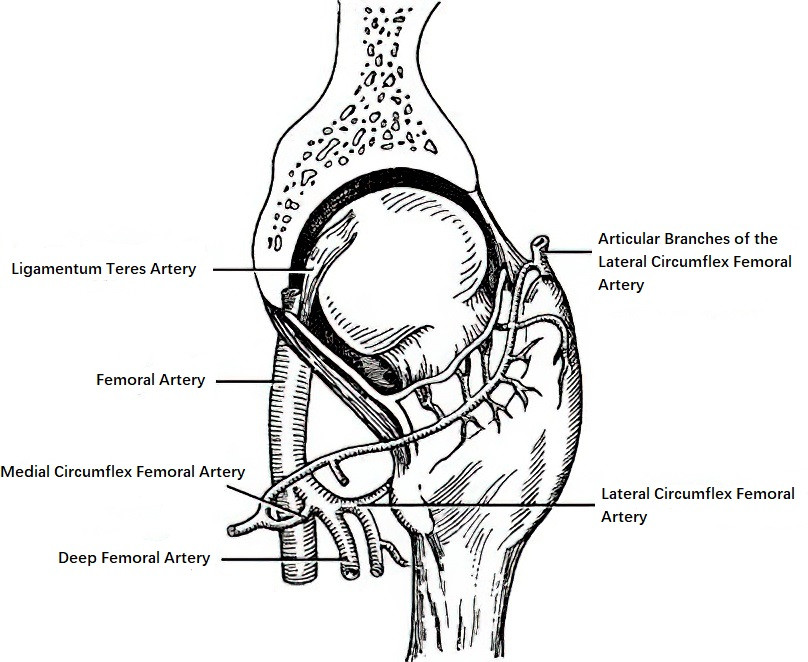
Figure 3 Blood supply to the femoral head
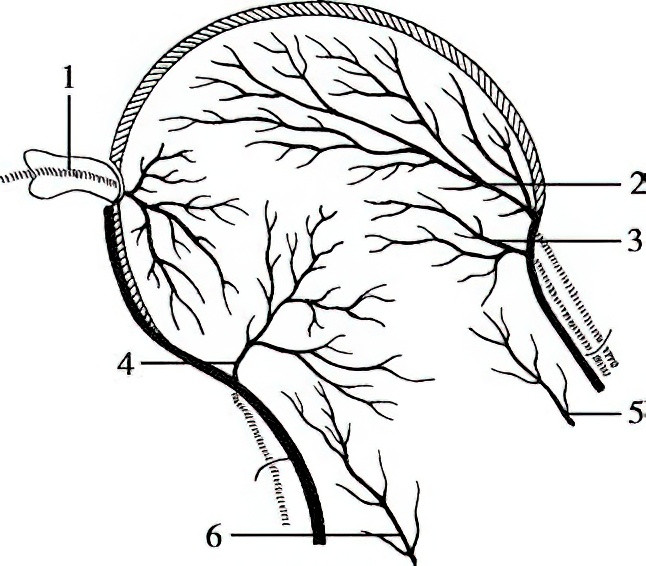
Figure 4 Blood supply of the femoral head
1, Foveal Artery
2, Lateral Epiphyseal Artery
3, Superior Metaphyseal Artery
4, Inferior Metaphyseal Artery
5, 6, Nutrient Artery Ascending Branches
Etiology and Classification
Fractures of the femoral neck account for 3.6% of fractures in adults, with the majority occurring in middle-aged and elderly individuals. These fractures are often associated with decreased bone mass resulting from osteoporosis, whereby even minor torsional forces can lead to fractures. In most cases, such fractures occur when individuals fall while walking, causing a twisting motion that results in indirect trauma to the femoral neck. Femoral neck fractures in adolescents are relatively rare and typically require significant force, with unstable fracture types being more common.
Classification by Fracture Line Location
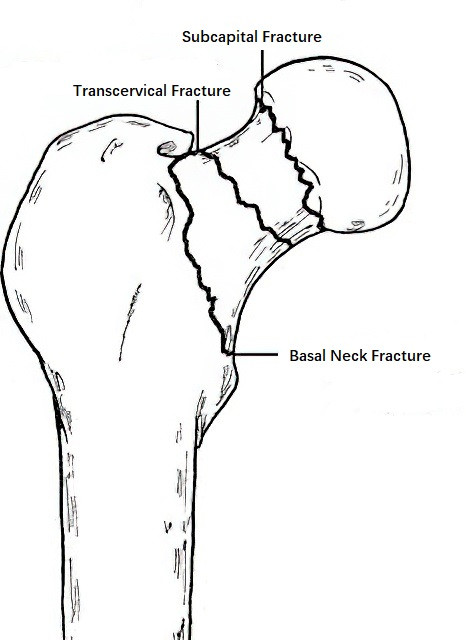
Figure 5 Classification by fracture location
Subcapital Fractures
The fracture line is located below the femoral head. Since the femoral head receives only minimal blood supply from the artery within the ligamentum teres femoris, there is significant risk of ischemia, making the occurrence of avascular necrosis highly likely.
Transcervical Fractures
The fracture line is located in the middle of the femoral neck. Blood supply to the femoral head is also markedly reduced in this type, increasing the likelihood of avascular necrosis or nonunion of the fracture.
Basal Neck Fractures
The fracture line is located at the junction of the femoral neck and the line connecting the greater and lesser trochanters. Due to the arterial ring formed at the base of the femoral neck by anastomoses of branches from the medial and lateral circumflex femoral arteries, blood supply to the fracture site is less disrupted, making these fractures more likely to heal.
Classification by Fracture Line Direction
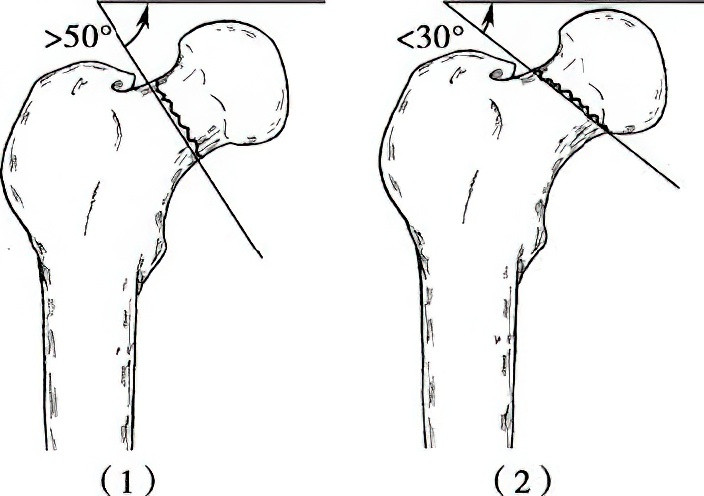
Figure 6 Classification by fracture line direction
Adduction Fractures
The angle (Pauwels angle) between the distal fracture line and the line connecting the two iliac crests is greater than 50°, classifying it as an adduction-type fracture. These fractures have smaller contact surfaces and are prone to redisplacement, making them unstable fractures. The larger the Pauwels angle, the greater the shear force experienced by the fracture ends, further decreasing stability.
Abduction Fractures
The angle between the distal fracture line and the line connecting the two iliac crests is less than 30°, classifying it as an abduction-type fracture. With larger contact surfaces, these fractures are less likely to redisplace and are considered stable fractures. However, improper management, such as excessive traction, external rotation, adduction, or premature weight-bearing, may still cause displacement, converting them into unstable fractures.
Classification by Displacement Level
The Garden classification is a commonly used system based on the degree of fracture displacement observed on an anteroposterior X-ray of the proximal femur.
- Type I (Incomplete Fracture): There is partial disruption of bone integrity, or the fracture may be impacted.
- Type II (Complete Fracture without Displacement): The bone fracture is complete, but no displacement is observed.
- Type III (Complete Fracture with Partial Displacement): The fracture is complete, with partial displacement, though contact remains between the femoral head and femoral neck.
- Type IV (Complete Displacement Fracture): The fracture displays complete displacement.
Garden Types I and II account for 21.8% of femoral neck fractures, while Types III and IV account for 78.2%. Recent research has confirmed that fractures diagnosed as Garden Type I incomplete fractures using plain X-rays are often found to be complete fractures upon further examination with CT scans. Therefore, incomplete fractures in adults classified as Garden Type I do not actually exist.
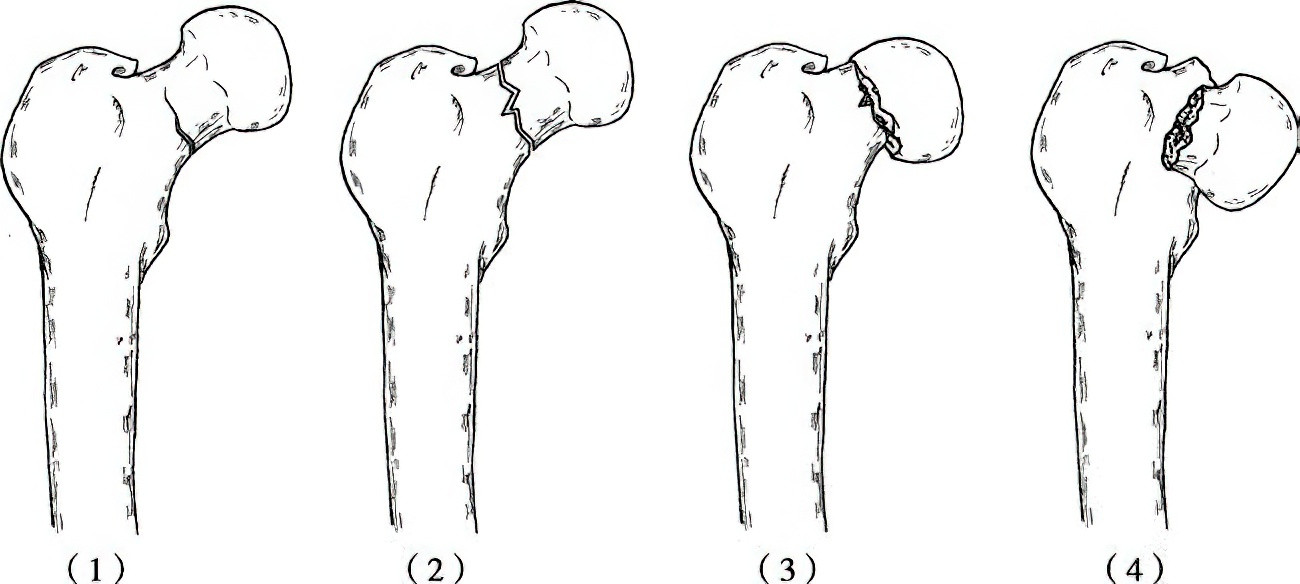
Figure 7 Garden classification for displacement:
(1) Type I: Incomplete or Impacted Fracture
(2) Type II: Complete Fracture Without Displacement
(3) Type III: Complete Fracture with Partial Displacement
(4) Type IV: Complete Fracture with Complete Displacement
Variations in factors such as the degree of force, angle of torsion, and systemic conditions can result in diverse fracture patterns. Even when X-rays suggest a stable fracture, such as an abduction type, or when no obvious displacement is observed—or even in impacted fractures considered stable—handling during transportation, early turning of the body during conservative treatment, or improper fixation postures may cause stable fractures to become unstable or lead to displacement in previously undisplaced fractures.
Clinical Manifestations and Diagnosis
In middle-aged or elderly individuals with a history of falls resulting in injury, the presence of hip pain, restricted mobility of the lower limb, and inability to stand or walk suggests the possibility of a femoral neck fracture. Occasionally, mobility impairment may not be immediately apparent after the injury, allowing individuals to walk temporarily. However, several days later, hip pain may worsen progressively, particularly after activity, eventually rendering the individual unable to walk. This progression indicates that the initial injury might have been a stable fracture, which later evolved into an unstable fracture, leading to functional impairment. Upon examination, the affected limb often manifests an external rotation deformity, typically between 45° and 60°. This deformity occurs because the distal end of the fracture loses stability provided by the joint capsule and the iliofemoral ligament, combined with the pulling forces of the gluteus medius, gluteus minimus, gluteus maximus (attached to the greater trochanter), and iliopsoas and adductor muscles (attached to the lesser trochanter). If external rotation deformity reaches 90°, the possibility of an intertrochanteric fracture should be considered.
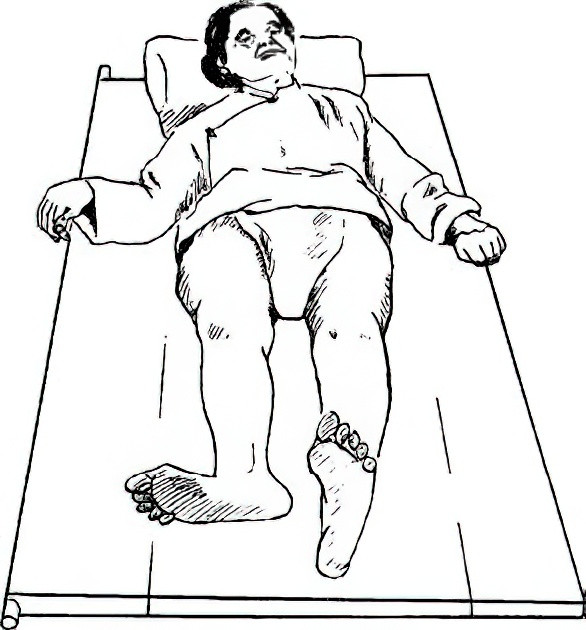
Figure 8 External rotation deformity in femoral neck fractures
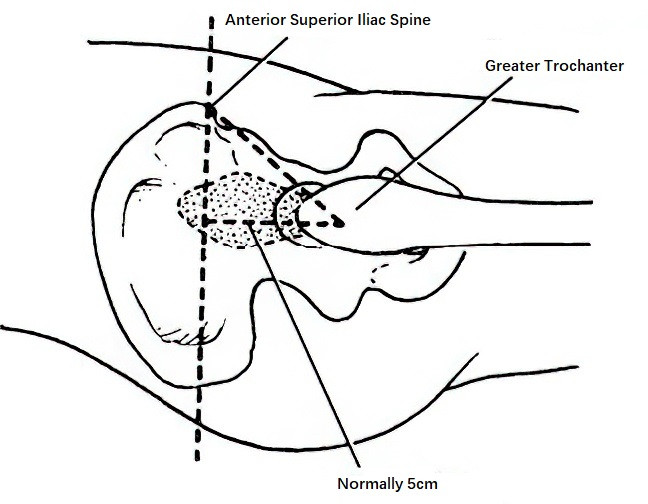
Figure 9 Bryant triangle
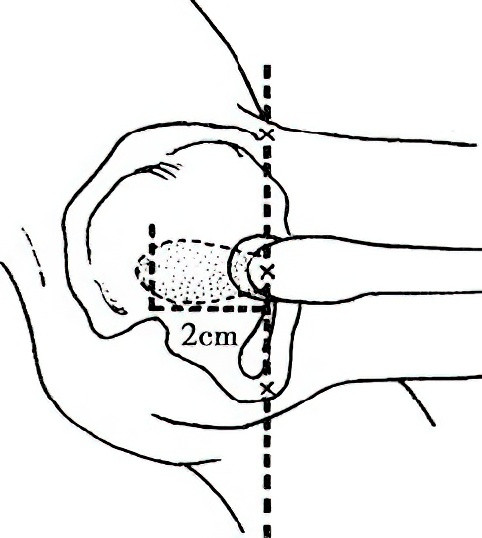
Figure 10 Nélaton’s line
Hip swelling and bruising are rarely observed after a femoral neck fracture, although localized tenderness and axial percussion pain may be present. Measurement of the affected limb may reveal limb shortening. In the supine position, drawing a perpendicular line from the anterior superior iliac spine to the bed surface, another horizontal line from the greater trochanter intersecting the perpendicular line, and a line connecting the anterior superior iliac spine to the greater trochanter form the Bryant triangle. In cases of femoral neck fractures, the base of this triangle is shortened compared to the unaffected side. When the patient is in a lateral position with the hip partially flexed, the line drawn between the anterior superior iliac spine and the ischial tuberosity is known as Nélaton's line. Normally, the greater trochanter is located on this line. If the greater trochanter lies above this line, it indicates upward displacement of the greater trochanter.
X-ray examination is essential for confirming the location, type, and displacement of the fracture, and it serves as a critical basis for selecting treatment. Anteroposterior X-rays of the hip do not clearly reveal anterior or posterior displacement of the fracture, necessitating the use of lateral views to accurately assess displacement.
Treatment
For patients of advanced age with poor general health or severe cardiac, pulmonary, renal, or hepatic dysfunction, who are unable to tolerate surgery, efforts should focus on promptly preventing and managing systemic complications. Surgery should be performed as soon as overall health permits. For patients who can undergo surgery within 24 hours, use of anti-rotation shoes may be sufficient during the waiting period. For those unable to undergo surgery within 24 hours, skin traction or tibial tuberosity traction is recommended, with traction weight ranging from 1/11 to 1/7 of the patient’s body weight. Isometric quadriceps contraction exercises and ankle and toe flexion-extension movements are advised to prevent venous stasis or deep vein thrombosis.
Surgical Methods
Closed Reduction and Internal Fixation
Under epidural anesthesia, the patient is placed in a supine position on an orthopedic traction table or uses a dual-countertraction reduction device. Once reduction is successfully achieved, three cannulated compression screws are inserted minimally invasively, or a dynamic hip screw is used for fixation. If rotation of the femoral head is observed during screw insertion, combined application of cannulated compression screws and dynamic hip screws may be necessary. For cases where conventional closed reduction fails, intraoperative three-dimensional reduction techniques involving interaction between the femoral head and shaft are encouraged to avoid open reduction whenever possible.
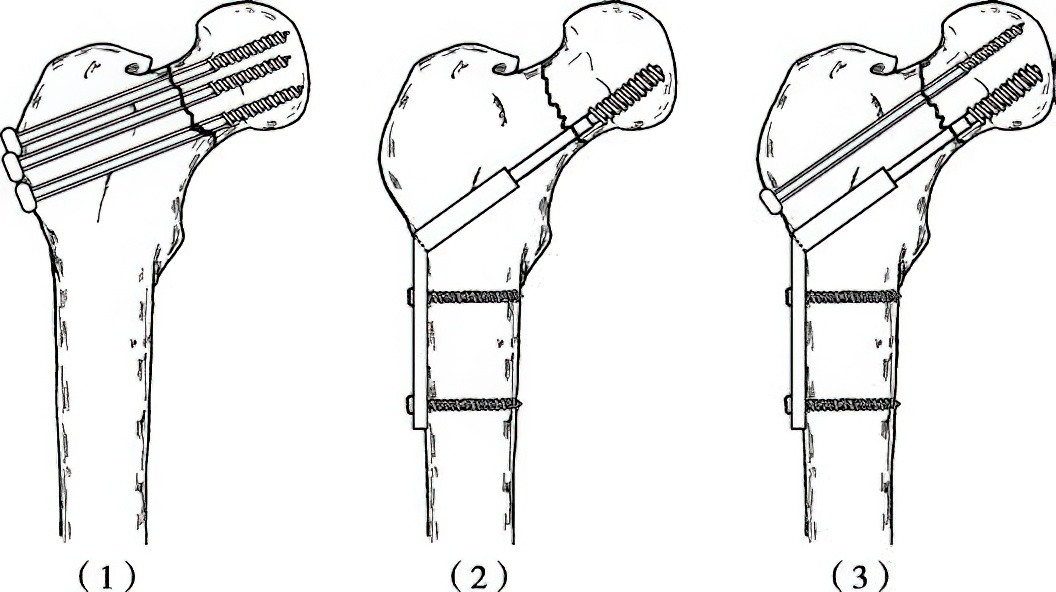
Figure 11 Internal fixation techniques for femoral neck fractures
(1) Cannulated Compression Screw Fixation
(2) Dynamic Hip Screw Fixation
(3) Combined Fixation Using Cannulated Compression Screws and Dynamic Hip Screws
Open Reduction and Internal Fixation
Cases where closed reduction fails or nonunion occurs in old fractures in young or middle-aged individuals necessitate open reduction and internal fixation. Through an anterolateral approach, the fracture site is exposed, and sclerotic tissue at the fracture ends is removed. Under direct vision, cannulated screws are inserted below the greater trochanter. Iliac bone grafts with vascular pedicles, such as those based on the deep circumflex iliac artery, the ascending branch of the lateral circumflex femoral artery, or the sartorius muscle pedicle, can also be used to promote fracture healing and prevent avascular necrosis of the femoral head. If a posterolateral approach is used, bone grafting using fragments with quadratus femoris pedicles is applicable.
Arthroplasty
For elderly patients with Garden III or IV femoral neck fractures and relatively good overall condition and life expectancy, total hip replacement is recommended. For elderly patients with poor overall health, multiple comorbidities, and shorter life expectancy, hemiarthroplasty is preferred.
Postoperative Management
After internal fixation using cannulated screws, patients with normal bone mass, anatomical reduction, and stable fixation can sit up in bed and actively move their knees and ankles but should avoid side-lying or cross-legged positions. Partial weight-bearing with the assistance of two crutches may begin at six weeks, progressing to full weight-bearing upon fracture healing.
For patients undergoing hemiarthroplasty or total hip replacement, hip flexion-extension exercises and active quadriceps contraction training should commence postoperatively. Depending on the patient’s systemic condition and tolerance, assisted mobilization as early as 24 hours post-surgery may be initiated. By the first postoperative week, patients may begin walking with the aid of walkers.