Mechanism of Dislocation
Posterior hip dislocation most commonly occurs in traffic accidents. When a seated individual is in a position of knee flexion combined with hip flexion, adduction, and slight internal rotation, an impact to the knee can cause the femoral head to dislocate through the posterior-inferior weak area of the hip joint capsule.
Classification
Clinically, the Epstein classification method is frequently used, which divides posterior hip dislocations into five types:
- Type I: Simple dislocation or dislocation accompanied by a small fracture fragment of the posterior wall of the acetabulum.
- Type II: Dislocation of the femoral head combined with a large fracture of the posterior wall of the acetabulum.
- Type III: Dislocation of the femoral head accompanied by comminuted fracture of the posterior wall of the acetabulum.
- Type IV: Dislocation of the femoral head accompanied by fractures involving both the posterior wall and the superior aspect of the acetabulum.
- Type V: Dislocation of the femoral head accompanied by a fracture of the femoral head itself.
Clinical Presentation and Diagnosis
A significant history of trauma, generally involving substantial force, such as a car accident or a fall from height, is present.
Severe pain and inability to actively move the hip joint are present.
The affected limb appears shortened, with the hip joint presenting in flexion, adduction, and internal rotation deformity.
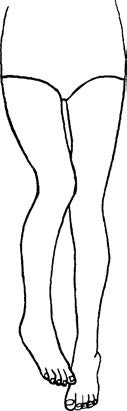
Figure 1 Typical deformity of posterior hip dislocation
The dislocated femoral head can be palpated in the gluteal region, and the greater trochanter is markedly elevated.
Posterior hip dislocations may be associated with sciatic nerve injury, which occurs in approximately 10% of cases. Patients with sciatic nerve involvement often show symptoms primarily of common peroneal nerve damage, such as foot drop, weakness in dorsiflexion of the toes, and sensory deficits on the lateral dorsum of the foot. These are generally caused by temporary functional impairment due to nerve traction or mild contusion by the dislocated femoral head or acetabular fracture fragments. Most patients recover gradually after the injury. However, if no recovery is observed after 2–3 months, surgical exploration should be considered.
X-rays can provide information about the dislocation as well as the presence of fractures. CT may be necessary to assess the displacement of fracture fragments.
Treatment
Treatment of Type I Injuries
Reduction
Reduction of the dislocated hip joint requires muscle relaxation, which must be achieved under general anesthesia or spinal anesthesia. Early reduction is recommended. The first 24–48 hours represent the optimal time for successful reduction, with the procedure ideally completed within 24 hours. Reductions performed in 48–72 hours become significantly more challenging, with increased complications and a marked decline in joint function. The commonly used reduction technique is the Allis method (traction-lift technique). In this method, the patient is placed in the supine position. An assistant crouches beside the patient, using both hands to stabilize the iliac crests and fix the pelvis. The surgeon stands facing the patient, flexing the hip and knee joints to 90°. The surgeon then grasps the popliteal fossa with both hands and applies sustained traction, or alternatively loops the upper forearm around the popliteal fossa for traction. Once muscle relaxation is achieved, slight external rotation of the limb allows the femoral head to reposition within the acetabulum. A distinct "clunk" accompanied by bouncing sensation suggests successful reduction. Following reduction, the deformity resolves, and hip joint mobility is restored. This method is straightforward, safe, and widely utilized.

Figure 2 Allis method
Immobilization and Functional Training
After reduction, bandages are used to temporarily bind the patient's ankles together, and the patient is transported to bed with the hip extended. The affected limb is placed in skin traction or a T-shaped splint for 2–3 weeks. During bed rest, the quadriceps should be kept active with isometric exercises. Joint mobility exercises are initiated after 2–3 weeks. Weight-bearing with assistance (e.g., using crutches) begins after 4 weeks. Full weight-bearing is typically resumed by 3 months.
Treatment of Type II–V Injuries
For complex posterior hip dislocations, current treatment approaches remain a subject of debate. However, considering the high likelihood of intra-articular fractures leading to post-traumatic osteoarthritis, early open reduction and internal fixation are generally favored.