A completely severed limb (finger) refers to a traumatic detachment of the limb (finger) with no remaining tissue connection, or cases where the attached tissue is necrotic and must be removed during debridement. This is classified as a complete severance. An incompletely severed limb (finger) refers to cases where the severance involves major vascular rupture with fracture-dislocation, the amount of soft tissue connecting the severed limb (finger) is less than 1/4 of the cross-sectional area, and the connected skin is less than 1/8 of the circumference. Without vascular anastomosis, necrosis of the distal part of the limb (finger) will occur, which defines incomplete detachment.
Emergency Measures for Severed Limbs (Fingers)
Emergency care includes hemostasis, dressing, immobilization, preservation of the severed limb (finger), and rapid transportation. These measures are similar to emergency care for hand injuries.
The severed end of the limb (finger) should be wrapped in clean dressing to minimize contamination. If the injury occurs far from a hospital, the severed limb (finger) should be preserved using the dry-cooling method. The limb (finger) should be wrapped in clean, dry, non-medicated dressing, placed in a sealed plastic bag, and put into a container with a lid, with ice blocks placed around the container. Direct soaking of the severed limb (finger) in any liquid should be avoided. Upon arrival at the hospital, the severed limb (finger) should be inspected, wrapped in sterile dressing, placed in a sterile tray, and stored in a refrigerator at 4°C.
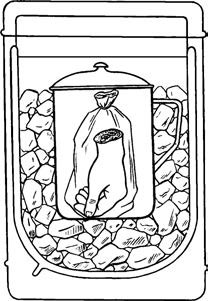
Figure 1 Preservation method for severed hand
Indications and Contraindications
General Condition
A stable general condition is a prerequisite for replantation. In cases of complex or multiple injuries, the primary focus should be on saving the patient’s life. The severed limb (finger) should be stored in a 4°C refrigerator to wait for replantation until vital signs stabilize.
Extent of Limb Injury
The extent of injury depends on the nature of the trauma. Injuries caused by sharp objects result only in tissue severance at the detachment plane, producing clean cuts with minor contamination and minimal damage to critical structures, making survival rates for replantation high. Crush injuries cause severe tissue damage, but when the damage is confined to a limited area, removing the crushed tissue and shortening the affected limb (finger) slightly still yields a high survival rate for replantation. In contrast, avulsion injuries involve extensive tissue damage. Blood vessels, nerves, and tendons may be avulsed at different planes, often requiring complex vascular grafting. Replantation following such injuries has a lower success rate, and even when successful, functional outcomes may be poor.
Level of Severance and Timing of Replantation
The sooner replantation surgery is performed, the higher the likelihood of success. Generally, surgery should be performed within 6–8 hours of injury. Early cooling or cold weather conditions may extend this time frame. The time limit for replantation is closely related to the level of severance. For severed fingers, because of their unique tissue composition, the procedure may be delayed up to 12–24 hours. High-level severances, however, involve muscle-rich tissues, where ischemia for more than 6–7 hours at room temperature causes muscle cell necrosis. This leads to the release of toxic substances like potassium ions, myoglobin, and peptides, which accumulate in the tissue fluid and blood of the severed limb. When replantation is performed, these toxic substances can cause systemic toxicity, potentially leading to death due to reperfusion injury. For this reason, replantation of high-level amputations is strictly limited to within 6–8 hours.
Age
There is no direct causal relationship between age and limb (finger) replantation. However, in elderly patients with poor physical condition or chronic systemic illnesses, replantation should be carefully considered.
Contraindications for Replantation
Replantation is strictly contraindicated in any of the following circumstances:
- Patients with systemic chronic diseases, severe visceral organ damage, inability to withstand prolonged surgery, bleeding tendencies, or poor general condition.
- Severed limbs (fingers) with multiple fractures, severe soft tissue crush injuries, extensive damage to the vascular bed, high-level avulsions of blood vessels, nerves, and tendons, with expected poor postoperative functional recovery.
- Severed limbs (fingers) soaked in irritating solutions or disinfectants for extended periods.
- Severed limbs (fingers) left for too long without proper cold storage, especially in high-temperature conditions.
- Patients with mental disorders, unwillingness to cooperate with postoperative care, or lack of desire for replantation.
Surgical Principles
Replantation of severed limbs (fingers) represents a comprehensive application of various techniques in trauma surgery. It requires the surgeon to have a solid foundation in surgical principles and proficient microsurgical skills to ensure the survival of the replanted limb (finger). If the limb (finger) has been severed for a short period, it should be repaired following a specific sequence: fracture fixation, repair of flexor and extensor tendons, venous and arterial anastomosis, nerve repair, and wound closure. If the duration of severance is prolonged, arterial and venous anastomosis should follow fracture fixation first to minimize the time of tissue ischemia, after which other tissues can be repaired. The basic principles and procedures are outlined below.
Thorough Debridement
Debridement is both a critical step in the surgery and a further assessment of the condition of the severed limb (finger). Typically, two surgical teams work simultaneously to perform debridement on both the proximal and distal ends of the severed limb (finger). Blood vessels, nerves, and tendons should be carefully identified, trimmed, and marked.
Reshaping and Rebuilding the Bone Framework
To reduce tension on vascular and neural sutures, bones may be appropriately trimmed and shortened. Fracture fixation should be simple, quick, minimally invasive, reliable, and conducive to healing. Various methods of internal or external fixation can be applied as appropriate to the situation.
Suturing of Muscles and Tendons
After rebuilding the bone framework and before vascular anastomosis, muscles and tendons are sutured under appropriate tension. This approach establishes a favorable tissue bed for vascular anastomosis and helps adjust vascular tension. At the same time, this reduces irritation and stress on the vascular anastomosis sites. The selection of muscle and tendon sutures should focus on restoring hand function, and not all tendons need to be sutured. For example, in the distal forearm, the flexor pollicis longus, flexor digitorum profundus, wrist flexors, extensor pollicis longus, abductor pollicis longus, extensor digitorum communis, and wrist extensors should be sutured, while other tendons may be left unsutured. For finger replantation, the flexor digitorum profundus tendon and extensor tendon should be restored.
Reconstruction of Blood Circulation
The arteries and veins should undergo debridement until healthy tissue is reached, followed by tension-free anastomosis. In cases of vascular defects, vascular transposition or grafting may be necessary. Anastomosis should restore the primary blood vessels, such as the ulnar and radial arteries or the paired proper digital arteries of the fingers. The number of anastomosed blood vessels should be maximized, with an optimal ratio of 1 artery to 2 veins. Generally, venous anastomosis is performed first, followed by arterial anastomosis.
Nerve Repair
Nerve repair should be performed during the first stage whenever possible. The epineurium should be sutured in a tension-free state. If a nerve defect exists, nerve grafting may be required.
Wound Closure
After replantation of the severed limb (finger), the wound should be closed whenever possible. If primary closure is not feasible, negative pressure wound therapy may be applied. Potential issues for closure should be thoroughly evaluated during debridement. To prevent the formation of circular scars during skin suturing, a Z-plasty technique can be employed to convert straight incisions into curved ones. If there is a skin defect, a medium-thickness or full-thickness skin graft, or a local flap transfer, may be used for coverage.
Dressing and Immobilization
The blood stains should be cleaned using warm saline, and the wound should be dressed with multiple layers of soft sterile dressings. Fingers should be separated, leaving the fingertips exposed to monitor distal blood circulation. The wrist should be immobilized in a functional position using a plaster splint. The extent of immobilization should accommodate the level of amputation, ranging from the fingertips to the forearm, or even extending beyond the elbow joint.
Postoperative Management
General Care
The ward environment should remain quiet, comfortable, and well-ventilated, with room temperature maintained between 20–25°C. The affected limb should be elevated above heart level. A 60W floor lamp should provide localized illumination, with a distance of 30–50 cm from the limb to aid in blood circulation and localized warming. However, excessive proximity to the light source can risk burns. Bed rest should be maintained for about 10 days, with cold exposure strictly avoided. Smoking by the patient or others in the room should be strictly prohibited to prevent vascular spasms.
Close Monitoring of Systemic Reactions
Systemic reactions are usually mild after replantation of low-level severed limbs (fingers). High-level limb replantation, especially following prolonged ischemia, may result in complications beyond hypovolemia-induced shock and poor blood circulation in the replanted limb. These complications can include cardiotoxicity, nephrotoxicity, or neurotoxicity, manifesting as persistent high fever, restlessness, or even coma. Symptoms such as tachycardia, weak pulses, hypotension, hemoglobinuria, reduced urine output, or anuria should be addressed promptly. If systemic conditions fail to improve or become life-threatening, the replanted limb must be amputated in a timely manner.
Routine Observation of Blood Circulation in the Replanted Limb (Finger)
Within 48 hours postoperatively, arterial insufficiency or venous outflow obstruction may commonly occur in the replanted limb (finger). Monitoring should be performed every 1–2 hours, comparing the affected side with the unaffected side, and detailed records should be maintained. Under normal conditions, the replanted limb (finger) appears full at the pulp, with a reddish complexion, slight warmth compared to the unaffected side, and good vitality demonstrated by a capillary refill time of 1–2 seconds. When the side of the fingertip is incised, bright red blood should flow within 1–2 seconds. Signs of arterial interruption (arterial crisis) include pale skin, decreased skin temperature, absent capillary refill, shriveled fingertip pulp, and no blood flow from incisions. Causes commonly include vascular spasms or thrombosis at the anastomosis site. When arterial crisis is suspected, dressings should be loosened, and compressive factors eliminated. Cervical or epidural anesthesia, along with antispasmodic medications such as papaverine or anisodamine (654-2), and hyperbaric oxygen therapy, may be applied. If symptoms fail to improve after brief observation, immediate surgical exploration may be necessary to remove thrombi, excise the affected anastomosis site, and perform reanastomosis to ensure limb survival.
Signs of venous outflow obstruction (venous crisis) include a transition from a reddish to a dark red fingertip, increased pulp tension, accelerated capillary refill, and decreased skin temperature. When the fingertip is incised, dark red blood flows out. Prolonged venous crisis can lead to arterial crisis, jeopardizing the survival of the replanted limb (finger). To address venous crisis, compressive factors should be removed, and fingertip incisions made to allow blood drainage. Surgical exploration may be required if necessary.
Prevention of Vascular Spasms and Anticoagulation Therapy
Measures such as keeping the patient warm, providing analgesia, and prohibiting smoking should be adopted to minimize vascular spasms. Continuous brachial plexus or epidural anesthesia via catheterization with periodic anesthetic injections can provide analgesia while maintaining vascular dilation and preventing spasms. Anticoagulants and antispasmodic drugs, such as dextran-40 (500 ml intravenously twice daily for 5–7 days in adults, with reduced doses in children), may be used. Low-molecular-weight heparin injection may also be administered.
Antibiotic Use
In cases where severed limbs (fingers) are heavily contaminated or surgeries are prolonged, antibiotics should be administered to prevent infections.
Rehabilitation of Replanted Limbs (Fingers)
After fracture healing and removal of external fixation, active and passive functional training should be initiated, supplemented by physical therapy to promote functional recovery. If tendon adhesions occur, tenolysis should be performed. Secondary repair of nerves or tendons should be performed as early as possible if necessary.