The ability of the hand to perform functions such as grasping, holding, pinching, and gripping is intricately based on its complex anatomy and refined structural organization. Hand injuries, caused by various factors, may leave scars in mild cases or lead to functional impairment and even loss in severe cases. As a result, early and accurate diagnosis, along with timely and effective treatment, is particularly important.
Applied Anatomy
Relevant anatomy can be found in associated anatomical references. Here, only hand postures related to the diagnosis and treatment of hand injuries are discussed. The normal hand posture includes the resting position and the functional position.
The resting position of the hand is the state in which the tension of the intrinsic and extrinsic muscles, joint capsules, and ligaments is relatively balanced, representing the natural state of the hand at rest. It is characterized by the wrist joint dorsiflexed at 10°–15°, with slight ulnar deviation; the metacarpophalangeal and interphalangeal joints are in partial flexion, with the distance between the fingertips and the palm gradually decreasing from the index finger to the small finger. The extended axes of the fingers converge at the scaphoid tubercle. The thumb is slightly abducted, with its pulp facing the radial side of the distal interphalangeal joint of the index finger. Clinically, it is significant because the resting position of the hand changes following tendon injuries.

Figure 1 Resting position of the hand

Figure 2 Functional position of the hand
The functional position of the hand is a preparatory posture that facilitates functional use, resembling the position of holding a ball. It is characterized by the wrist joint dorsiflexed at 20°–25°, with slight ulnar deviation. The thumb is abducted and externally rotated, in opposition to the remaining fingers, with its metacarpophalangeal and interphalangeal joints slightly flexed. The other fingers are slightly spread apart, with the metacarpophalangeal and proximal interphalangeal joints in a semi-flexed position, and the distal interphalangeal joints slightly flexed. The degree of flexion is relatively consistent across all finger joints. Clinically, this position is significant for postoperative care following severe hand injuries. Particularly in cases where joint function is not expected to fully recover or joint ankylosis is likely to occur, fixing the hand in this position allows for the preservation of maximum functional capacity.
Causes and Characteristics of Injuries
Puncture Wounds
Caused by sharp objects such as nails, needles, or bamboo splinters, these injuries typically present as small, deep wounds that may introduce contaminants into deep tissues, leading to infections. They carry risks of nerve and vascular damage and are prone to being missed during diagnosis, thus requiring high clinical vigilance.
Laceration Injuries
These result from sharp objects like knives, glass, or power saws. The wounds often have clean edges with mild contamination. These injuries may sever blood vessels, nerves, or tendons, and severe cases may result in amputated fingers or palms.
Blunt Force Injuries
These are caused by impacts from hammers, heavy objects, or crushing forces. Such trauma may split or avulse the skin, damage nerves, tendons, and blood vessels, and in extreme cases, lead to catastrophic hand destruction.
Crush Injuries
These injuries manifest differently depending on the causative object. For example, door or window compression may cause subungual hematomas, nail bed lacerations, or distal phalanx fractures. Heavy machinery or rolling equipment can induce extensive skin avulsions or degloving injuries, often accompanied by deep tissue damage, multiple fractures, or even limb devastation.
Firearm Injuries
Resulting from explosives, firecrackers, or gunshots, these injuries are characterized by high-velocity impact, explosive force, and thermal burns. Wounds exhibit diverse patterns with extensive tissue destruction, heavy contamination, and significant necrotic tissue, making them highly susceptible to infection.
Examination and Diagnosis
Regardless of whether a hand injury is accompanied by other systemic injuries, during emergency visits, the principles of assessing both systemic and local conditions, examining systems and tissues, and prioritizing survival and function must be followed. Comprehensive, dynamic examinations should be performed to establish a complete diagnosis. This approach helps to prevent missed or incorrect diagnoses and ensures adequate mental and equipment preparation for treatment.
Examination of Skin Injuries
This includes evaluating the location and nature of the wound, determining whether deeper tissues are affected, and identifying whether there is a skin defect and the extent of such a defect. Assessing the viability of the skin following injury is particularly crucial. The nature of the injury significantly influences skin survival. For example, in incised wounds, the blood supply to the edges of the skin remains intact, making wound healing easier. Conversely, in crush injuries, skin can display extensive tearing or avulsion; in cases of subcutaneous degloving, despite intact overlying skin, its circulation from the underlying base is disrupted, potentially compromising viability. Methods for assessing skin viability include the following:
Skin Color and Temperature
Skin that matches the surrounding area indicates good viability, while skin that appears pale, cyanotic, or cold suggests poor viability.
Capillary Refill Test
When the skin is pressed to turn it white and then released, rapid return of redness indicates good viability. In normal tissue, redness returns within ≤2 seconds after pressure is removed. A delayed or absent return indicates poor or absent viability.
Bleeding at the Wound Edges
When the edges of the skin are wiped with sterile gauze or trimmed, pinpoint bright red bleeding indicates good viability. Lack of bleeding suggests poor viability.
Examination of Tendon Injuries
Rupture of flexor or extensor tendons in different planes of the hand may result in characteristic postural changes. First, the resting position of the hand may be altered: rupture of a flexor tendon increases the resting extension of the affected finger, while rupture of an extensor tendon increases its resting flexion. Imbalance between the flexor and extensor tendons leads to impaired active flexion and extension of the fingers. Tendon rupture in specific locations may cause distinct finger deformities. Rupture of both the flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) at the metacarpophalangeal joint results in the affected finger assuming a straight position. Extensor tendon rupture in this region leads to the finger being in a flexed position. Rupture of extensor tendons at the dorsal side of the proximal phalanx causes flexion at the proximal interphalangeal joint. Rupture at the dorsal side of the middle phalanx causes flexion of the distal interphalangeal joint, producing a mallet finger deformity. At the wrist joint, multiple tendons contribute to dorsiflexion and palmar flexion. Rupture of a single tendon may not result in significant functional deficits, but rupture of the FDP and FDS tendons may lead to flexion of the metacarpophalangeal joint due to interosseous and lumbrical muscle contraction.
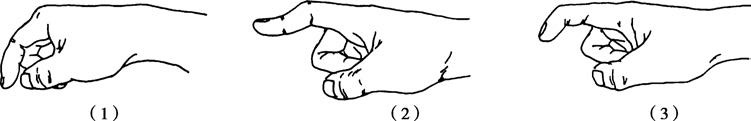
Figure 3 Methods for examining extensor tendons
1, Rupture of the extensor tendon at the dorsum of the metacarpophalangeal joint
2, Rupture of the extensor tendon at the dorsum of the proximal phalanx
3, Rupture of the extensor tendon at the dorsum of the middle phalanx
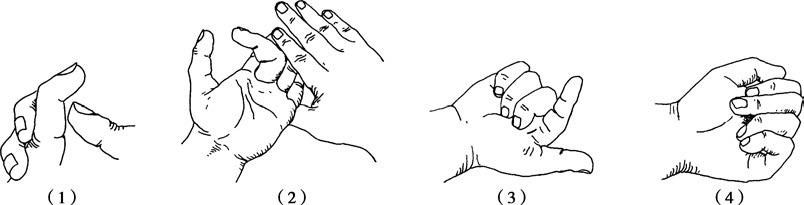
Figure 4 Methods for examining flexor tendons
1, Technique for examining the flexor digitorum profundus tendon
2, Technique for examining the flexor digitorum superficialis tendon
3, Rupture of both the flexor digitorum profundus and superficialis tendons
4, Rupture of the flexor digitorum profundus tendon
Examination of the FDP tendon involves fixing the proximal interphalangeal joint in extension and asking the patient to actively flex the distal interphalangeal joint. Inability to do so indicates FDP tendon rupture. Examination of the FDS tendon is performed by fixing the other three fingers in extension and asking the patient to actively flex the proximal interphalangeal joint of the affected finger. Inability to do so indicates FDS tendon rupture. If both the proximal and distal interphalangeal joints cannot be actively flexed, rupture of both the FDS and FDP tendons is indicated. Examination of the flexor pollicis longus tendon involves fixing the thumb's metacarpophalangeal joint in extension and asking the patient to flex the interphalangeal joint of the thumb.
Examination of Nerve Injuries
The terminal branches of the brachial plexus include the median, ulnar, and radial nerves, which control motor and sensory functions of the hand. Distally from the wrist, the median and ulnar nerves innervate intrinsic hand muscles and provide sensory functions, while the radial nerve supplies only sensory input.
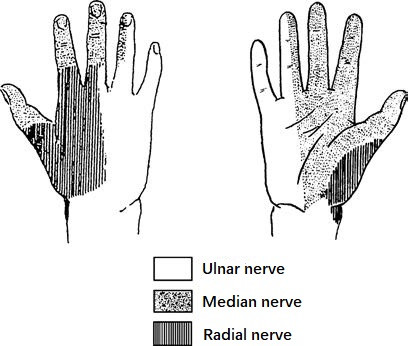
Figure 5 Distribution of sensory nerves in the hand
Median Nerve Injury
Motor impairment includes paralysis of the abductor pollicis brevis and opponens pollicis, resulting in loss of thumb abduction, opposition, and pinch functions involving the thumb and index finger. Sensory impairments involve the radial half of the palm, the radial side of the thumb, index, middle, and half of the ring fingers, as well as the dorsal area of the thumb up to the interphalangeal joint and the radial sides of the index, middle, and ring fingers distal to the proximal interphalangeal joints.
Ulnar Nerve Injury
Motor impairment includes paralysis of the 3rd and 4th lumbricals, causing claw deformity in the ring and little fingers, as well as paralysis of the interossei and adductor pollicis, leading to Froment's sign. Froment's sign is characterized by flexion of the proximal interphalangeal joint and hyperextension of the distal interphalangeal joint of the index finger, along with hyperextension of the metacarpophalangeal joint and flexion of the interphalangeal joint of the thumb during opposition. Sensory impairments involve the ulnar side of the palm, the ulnar side of the ring finger, and the little finger, both on the palmar and dorsal aspects.
Radial Nerve Injury
Sensory impairment involves the radial side of the dorsum of the hand and the proximal areas of the first two and a half digits up to the proximal interphalangeal joints.
Examination of Vascular Injuries
This includes assessing the color, temperature, capillary refill, and pulsations of the hand and fingers. Arterial injuries may present with pale skin, decreased skin temperature, collapsed finger pulp, delayed or absent capillary refill, and weakened or absent arterial pulsations. Venous insufficiency presents with cyanosis, swelling, accelerated capillary refill, and preserved arterial pulsations. As the ulnar and radial arteries form the superficial and deep palmar arches with rich collateral circulation, isolated injuries to the ulnar or radial arteries rarely cause ischemia in the fingers. The Allen test is one effective method to assess the patency of the ulnar and radial arteries. Specifically, the patient is instructed to make a tight fist. The examiner compresses the ulnar and radial arteries at the wrist. Once the patient relaxes their hand, the palm will appear pale. Releasing pressure from the ulnar artery should result in rapid reddening of the palm. Repeating the test by releasing the radial artery instead should produce the same results, indicating patency of both arteries. If results differ, anatomical variations or vascular obstruction may be present.
Examination of Bone and Joint Injuries
Bone and joint injuries should be evaluated in accordance with the general principles outlined in Chapter 60, "Overview of Fractures." X-ray imaging remains the most crucial diagnostic tool. In addition to standard anteroposterior and lateral views, special views, such as oblique or scaphoid positions, may be needed to avoid overlapping shadows. CT scans are useful for assessing complex carpal fractures, and MRI is suited for evaluating ligament injuries and triangular fibrocartilage complex (TFCC) damage.
During examination of hand joint motion, the joint in neutral zero-position is considered to be at 0°. Bilateral comparison should be made to account for normal variation. The range of motion differs across joints under normal conditions: wrist flexion ranges from 50°–60°, wrist extension 50°–60°, radial deviation 25°–30°, and ulnar deviation 30°–40°. Combining both palms while extending the wrists or both dorsal surfaces of the hands while flexing the wrists allows comparative assessment of wrist mobility.
For the thumb, flexion-extension at the carpometacarpal joint ranges widely but typically extends from 30°–40°, with some individuals achieving up to 90°. Thumb interphalangeal joints have a range of 80°–90°. Thumb abduction, defined as movement parallel to the palm's plane, reaches up to 90°, while adduction brings the thumb into contact with the radial side of the proximal phalanx of the index finger. Thumb opposition involves synchronizing the pulp of the thumb with that of the little finger.
For the fingers, flexion at the metacarpophalangeal joints is 80°–90°, with hyperextension 0°–20°; flexion at the proximal interphalangeal joints is 90°–100° with no extension; and flexion at the distal interphalangeal joints is 70°–90° with no extension. Finger abduction and adduction, defined as movement away from or toward the middle finger as the central axis, range from 30°–40°.
On-Site Emergency Care
The principles of on-site emergency care for hand injuries include hemostasis, wound dressing, local immobilization, and rapid transportation.
Hemostasis
Localized pressure dressing is the simplest and most effective method for controlling bleeding in hand injuries. It can be applied to stop bleeding from wounds and from severed ulnar or radial arteries at the wrist level. The use of arterial tourniquets above the wrist level is strictly prohibited, as overly tight or prolonged application of a tourniquet may lead to finger necrosis. In cases where the pressure is insufficient and only venous bleeding is blocked while arterial bleeding remains uncontrolled, bleeding may worsen.
Wound Dressing
Wounds should be dressed with sterile gauze or clean cloth to prevent further contamination. Solutions or antimicrobial medications should not be applied directly to the wound.
Local Immobilization
Materials readily available at the site, such as wooden boards, bamboo splints, or rigid cardboard, can be used for immobilization. The injured area should be fixed above the wrist level to reduce abnormal movements during transportation, alleviate pain, and prevent further tissue damage.
Rapid Transportation
The goal of rapid transportation is to secure the best possible timing for treatment.
Principles of Treatment
Early and Thorough Debridement
Although similar to the principles for open wounds and open fractures, the complexity of hand anatomy and the high functional demands of the hand make debridement particularly specific for hand injuries. Debridement should be performed under proper anesthesia and tourniquet control. It is carried out sequentially from superficial to deep layers, identifying and thoroughly cleaning all tissue types to prevent missed diagnoses and to facilitate repair while minimizing further tissue damage.
Tissue Repair
Whenever possible, repair of tendons, nerves, blood vessels, bones, and other tissues in the hand should be completed in the first stage following debridement. Ideally, repair should be conducted within 6–8 hours after injury. If the injury occurred more than 12 hours prior, or if the wound is heavily contaminated, tissue damage is extensive, or necessary conditions are lacking, repair may need to be delayed until 3 weeks later or performed in a second stage approximately 12 weeks later. Vascular injuries that affect the hand's blood circulation must be repaired immediately, while fractures and joint dislocations should promptly be reduced and fixed.
Primary Wound Closure
For lacerations, direct suturing of the skin may be performed. In cases of crush or avulsion injuries, the amount of tissue to be debrided depends on the assessment of skin viability. In the presence of skin defects, if the underlying soft tissue is healthy or surrounding soft tissue can adequately cover deeper vital structures, autologous skin grafting may be used. For cases where nerves, tendons, or bones and joints are exposed, flap transfer methods should be utilized for repair.
For a minority of severely contaminated wounds with prolonged injury durations or high infection risks, physiological saline-soaked gauze, negative pressure wound closure, or irrigation may be used after removing foreign bodies and necrotic tissue. The wound can then be reassessed after 3–5 days, followed by another round of debridement and delayed repair.
Postoperative Care
Postoperative immobilization should be tailored to the extent of tissue injury and repair. Tendon repairs typically require immobilization for 3–4 weeks, nerve repairs for 4 weeks, joint dislocations for 3 weeks, and fractures for 4–6 weeks. Sutures are usually removed 10–14 days after surgery, depending on wound healing. Once tissue healing is achieved, external fixation should be removed as early as possible to initiate both active and passive functional exercises. Physical therapy should also be incorporated to facilitate functional recovery.
Appropriate medical therapy should include the use of antibiotics, tetanus antitoxin, analgesics, and medications to improve circulation as needed.
Treatment Methods
Treatment of Hand Fractures and Dislocations
The ultimate goal is to restore the motor functions of the hand. The treatment principles include accurate fracture reduction, effective fixation, and early rehabilitation exercises.
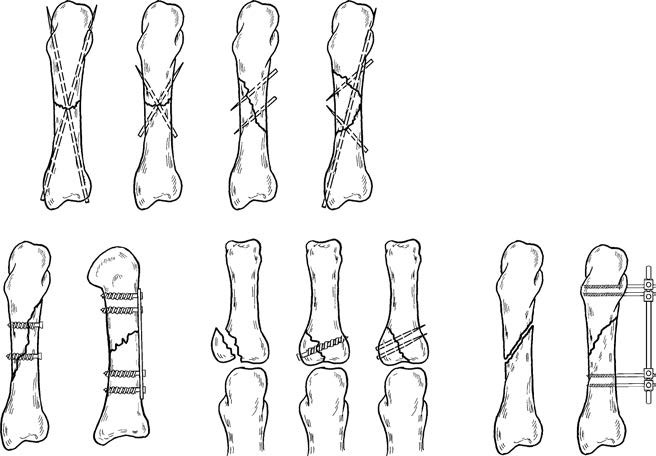
Figure 6 Internal fixation and miniature external fixation devices for metacarpal and phalangeal fractures
For open fractures and dislocations, regardless of wound conditions and injury severity, reduction should be performed immediately to restore blood supply to the affected hand or finger, protect vital blood vessels and nerves, and repair torn joint capsules and ligaments as early as possible. Common fixation methods for hand fractures include Kirschner wires, micro-plates with screws, and miniature external fixation devices.
Closed fractures without significant displacement, or fractures that are stable after reduction, can be treated non-surgically, with a fixation period of 4–6 weeks. Fractures of the distal phalanx usually show no significant displacement and generally do not require internal fixation. For comminuted fractures at the distal phalanx, treatment may focus on managing the soft tissue injury. If a subungual hematoma is present, puncturing the nail for drainage can relieve pressure and alleviate pain.
Repair of Tendon Injuries
Tendons serve as the transmission apparatus for joint movement. Tendon injuries can significantly impair hand function and should ideally be repaired in the first stage. The characteristics of tendon healing often result in adhesions after surgery, necessitating special techniques in suture methods and materials. Extensor tendons are surrounded by peritendinous tissue but lack tendon sheaths, resulting in relatively mild adhesions after surgery.
Flexor tendons, particularly those located between the middle third of the proximal phalanx and the distal palmar crease (from the insertion of the flexor digitorum superficialis on the middle phalanx to the origin of the tendon sheath at the metacarpophalangeal joint), form the so-called “no man’s land.” In this region, both the flexor digitorum profundus and flexor digitorum superficialis are covered by tendon sheaths. Tendon repairs in this area are prone to adhesions. In the past, excision of the flexor digitorum superficialis tendon was often recommended. However, advancements in the understanding of tendon healing mechanisms have led to the current practice of repairing both the flexor digitorum profundus and superficialis tendons in this region, along with concurrent repair of the tendon sheath.
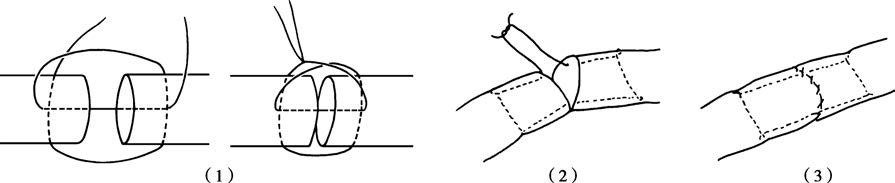
Figure 7 Tendon suturing techniques
1, Double-cross suture method
2, Kessler method
3, Modified Kessler method
Several techniques are used for tendon suturing, including the double-cross suture method, Kessler method, and modified Kessler method. In recent years, microsurgical techniques have become widely advocated to minimize damage to the tendon’s blood supply and promote tendon healing. After tendon suturing, immobilization is generally required for 3–4 weeks. During this period, active extension and passive flexion exercises for the fingers may be conducted under medical guidance. Once the tendon has healed, the fixation can be removed to initiate functional exercises, supplemented with physical therapy.
If adhesions develop, systematic rehabilitation therapy over 3–6 months may be required. If functional recovery remains poor, tendon release surgery may be necessary.
Repair of Nerve Injuries
Open nerve lacerations in the hand should be repaired in the first stage during debridement when appropriate conditions and technical expertise are available. If immediate repair is not feasible, the nerve ends should be secured with sutures during debridement, and repair can be postponed. Transfer to a higher-level medical facility should occur promptly, and repair should be performed in 2–3 weeks if the wound is free from infection.
In cases of severely contaminated wounds or associated skin defects, the epineurium at both ends of the severed nerve can be sutured to the surrounding tissues during debridement to prevent nerve retraction, facilitating delayed secondary repair.