An extension-type distal radius fracture (Colles fracture) commonly occurs when the wrist joint is in dorsiflexion, the palm contacts the ground, and the forearm is in pronation during injury.
Clinical Manifestations and Diagnosis
After injury, localized pain and swelling are present, often accompanied by a characteristic deformity. On lateral view, the deformity appears as a "dinner fork" (silver fork) shape, while on frontal view it resembles a "bayonet" deformity. There is significant tenderness at the site of the injury and impaired mobility of the wrist joint. X-ray imaging shows the distal fracture fragment displaced radially and dorsally, while the proximal segment is displaced volarly. These findings result in the typical deformity associated with this fracture. In addition, dislocation of the distal radioulnar joint and fracture of the ulnar styloid process may also be present.
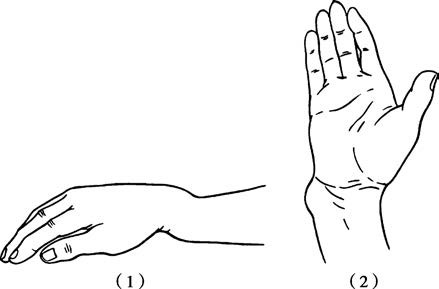
Figure 1 Deformities observed following extension-type distal radius fractures
(1) "Silver fork" deformity
(2) "Bayonet" deformity
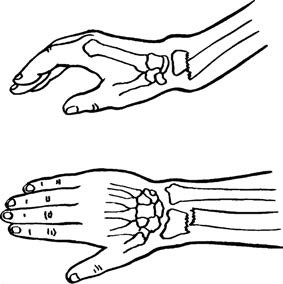
Figure 2 Typical displacement of fracture ends in extension-type distal radius fractures
Treatment
Treatment is primarily focused on closed reduction and external fixation, although surgical intervention may be required in certain cases.
Closed Reduction and External Fixation
With the shoulder abducted to 90 degrees, one assistant grips the thumb with one hand and the other fingers with the other hand, providing axial traction in the direction of the forearm's longitudinal axis. Another assistant applies counter-traction by stabilizing the proximal forearm near the elbow. After sufficient traction, the surgeon grasps the wrist with both hands, using the thumbs to push the distal fracture fragment distally and palmarly, while the other fingers stabilize and counterpressure the proximal fragment. The wrist angle is increased into flexion to correct the angulation, followed by gentle ulnar deviation pressure to realign the fragments. Traction is slowly released, and the reduction is checked under ulnar deviation and wrist flexion to evaluate alignment and stability. If the reduction is satisfactory, the forearm is immobilized using plaster. After swelling subsides in two weeks, the plaster cast may be replaced with either a neutral-position wrist splint or a tubular cast to immobilize the forearm until healing occurs.

Figure 3 Manual reduction for extension-type distal radius fractures
Open Reduction and Internal Fixation
Indications for surgery include:
- Severe comminuted fractures with significant displacement and articular surface involvement of the distal radius.
- Failure of closed reduction or successful reduction that cannot be maintained with external fixation.
Surgical Technique
A radial volar incision at the wrist is used to expose the fracture site. Under direct visualization, reduction is achieved and internal fixation is performed.
Rehabilitation
Regardless of whether closed reduction or open reduction is performed, early finger flexion and extension exercises should begin postoperatively. After external fixation is removed, gradual wrist exercises can be initiated. Following fracture healing, the dorsal surface of the distal radius may become uneven due to callus formation or suboptimal fracture alignment. This uneven surface can cause repetitive friction between the extensor pollicis longus tendon and the rough bone surface, leading to chronic injury and even spontaneous tendon rupture. Tendon transfer surgery can be performed to address this complication.
If uncorrected shortening deformity of the radius occurs, it may result in the ulnar bone appearing relatively elongated. This mismatch of joint surfaces at the distal radioulnar joint can cause chronic wrist pain and rotational limitations. Ulnar shortening osteotomy may be performed to correct these issues.