Anatomical Overview
The forearm consists of two bones: the ulna and the radius. The proximal end of the ulna, known as the olecranon, articulates with the trochlea of the humerus to form the ulnohumeral joint. The radial head of the radius articulates with the capitulum of the humerus, forming the radiocapitular joint. The proximal ends of the ulna and radius form the proximal radioulnar joint. The distal end of the ulna is the ulnar head, which, along with the triangular fibrocartilage, articulates with the proximal row of carpal bones to form the distal radioulnar joint. The distal end of the radius is enlarged and, together with the ulnar head, forms the radiocarpal joint with the proximal row of carpal bones. The distal ends of the ulna and radius also form the distal radioulnar joint. The interosseous membrane, a strong connective tissue, connects the ulna and radius along their lengths. Due to the natural curvature of both the ulna and radius, the distance between them varies, with the widest point measuring 1.5 to 2.0 centimeters. When the forearm is in a neutral position, the interosseous membrane is under the most tension; when the forearm rotates, the membrane becomes more relaxed. The fibers of the interosseous membrane run from the medial side of the ulna downward to the lateral side of the radius. In the event of a fracture in either the ulna or radius, the force can be transmitted through the interosseous membrane to the other bone, potentially causing a double fracture at different planes or resulting in a fracture of one bone with dislocation of the other. Both the ulna and radius have multiple muscles attached to their shafts, with origins and insertions distributed across various points. During a fracture, the pull of these muscles often leads to complex displacements, making reduction particularly challenging.
Etiology and Classification
Fractures of the shafts of the radius and ulna (fractures of radius and ulna) can result from direct, indirect, or torsional forces. In some cases, the combination of forces leading to the fracture is complex and difficult to analyze precisely.
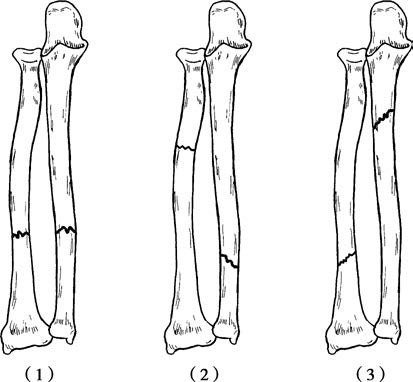
Figure 1 Types of double fractures of the radius and ulna shaft
1, Fractures caused by direct violence
2, Fractures caused by indirect violence
3, Fractures caused by rotational violence
Direct Trauma
This often occurs due to heavy objects striking the forearm, compression from machinery or vehicle wheels, or lacerations from sharp objects. These injuries typically result in transverse or comminuted fractures at the same plane. Direct force application frequently causes varying degrees of soft tissue damage, including muscle and tendon ruptures, as well as nerve and vascular injuries.
Indirect Trauma
When an individual falls with the palm striking the ground, the force is transmitted upward through the wrist joint. Since the radius bears more weight than the ulna, the radius is more likely to fracture first. If the remaining force is significant, it can be transmitted through the interosseous membrane to the ulna, causing a distal oblique fracture of the ulna.
Torsional Trauma
In cases where a fall results in the palm striking the ground while the forearm rotates, spiral or oblique fractures of the ulna and radius at different planes may occur. These fractures often involve a proximal ulna fracture and a distal radius fracture.
Clinical Manifestations and Diagnosis
After injury, the forearm exhibits pain, swelling, deformity, and functional impairment. Examination may reveal crepitus and abnormal joint-like motion at the fracture site. Bone conduction sound is reduced or absent. X-ray examination should include imaging of the elbow or wrist joint, as it can identify the exact location of the fracture, the type of fracture, the direction of displacement, and whether radial head dislocation or ulnar head dislocation is present. A fracture of the proximal one-third of the ulnar shaft may be associated with radial head dislocation, known as a Monteggia fracture. A fracture of the distal one-third of the radial shaft may be accompanied by ulnar head dislocation, referred to as a Galeazzi fracture.
Treatment
Closed Reduction and External Fixation
Improper treatment may lead to cross-union of the ulna and radius, which can impair rotational function. Therefore, the treatment goals include not only achieving proper alignment and positioning but also preventing deformities and rotation issues. In a position of shoulder abduction at 90 degrees and elbow flexion at 90 degrees, axial traction is applied along the forearm toward the distal end, with counter-traction applied at the elbow upwards. The traction position on the distal end depends on the fracture site.
If the fracture is above the insertion point of the pronator teres on the radius, the proximal fragment is often in a flexed and supinated position due to the pulling force of the supinator and biceps brachii, while the distal fragment is pronated due to the action of the pronator teres and pronator quadratus. In such cases, traction should be applied with the elbow slightly flexed and the forearm in a supinated position. If the fracture line is located below the insertion of the pronator teres, the balance between the supinator and pronator teres tends to place the proximal fragment in a neutral position, with the fracture site in slight pronation. Traction should then be applied with slight supination. For fractures in the distal third of the radius, the distal end is typically pronated due to the pull of the pronator quadratus, and traction should be applied in slight supination.
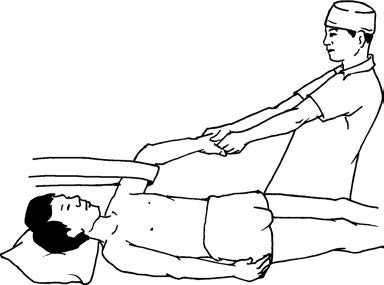
Figure 2 Manual reduction method for double fractures of the radius and ulna shaft
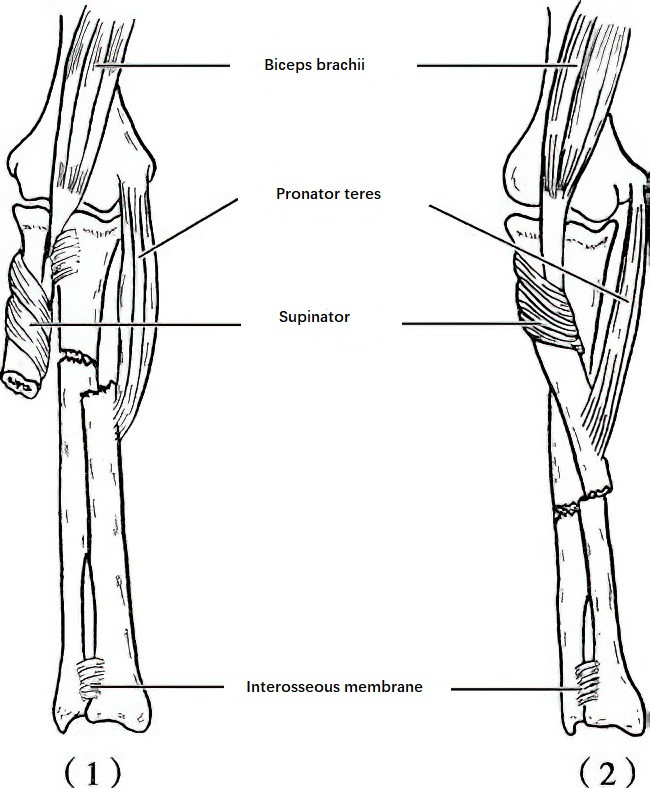
Figure 3 Displacement of double fractures of the radius and ulna shaft
1, Fracture of the upper 1/2 of the radius (above the attachment point of the pronator teres)
2, Fracture of the lower 1/2 of the radius (below the attachment point of the pronator teres)
After sufficient and sustained traction, rotational, shortening, and angulation deformities are corrected. The surgeon applies force with their thumbs and fingers on either side of the ulna and radius to separate the interosseous membrane, allowing reduction of the fracture ends. When necessary, further manipulation, such as angulation and counter-angulation, may be performed to complete the reduction. The following precautions should be considered during the procedure:
In double fractures, if one bone has a transverse stable fracture and the other a more unstable oblique or spiral fracture, the stable fracture should be reduced first. This stabilizes the bone through the interosseous membrane, making the reduction of the unstable fracture easier.
If both the ulna and radius fractures are unstable, reduction should prioritize the ulna in upper-third fractures, the radius in lower-third fractures, and generally the ulna in midshaft fractures. This is because the ulna is more superficial, with fewer muscular attachments and less severe displacement, making manual reduction relatively easier. Once one bone is reduced and stabilized, it facilitates reduction of the other.
In cases of oblique fractures facing away on X-ray, distal rotation of the fractured end should be suspected. Correction should first address the rotational displacement in the opposite direction, followed by reduction of the fracture ends.

Figure 4 Tubular plaster immobilization of the upper limb for double fractures of the radius and ulna
Once reduction is successful, plaster fixation is applied. Following successful closed reduction, anterior and posterior splints are used to immobilize the upper limb. After swelling subsides, tubular plaster casts are used to fix the upper limb. Bony union is generally achieved within 8-12 weeks.
Open Reduction and Internal Fixation
Indications for surgery include:
- Failure of closed reduction.
- Open fractures with minor wound contamination and a short injury-to-treatment interval.
- Associated nerve, vessel, or tendon injuries.
- Multiple injuries on the same limb.
- Malunion or ununited fractures.
Surgical Approach
The incision site should depend on the location of the fracture, typically requiring separate incisions over the ulna and radius along the intermuscular plane to fully expose the fracture ends. Accurate alignment is achieved under direct visualization, and fixation is performed using compressive plates or intramedullary nails. Care should be taken when using intramedullary nails due to the radial curvature of the bone.
Rehabilitation
Regardless of whether closed reduction with external fixation or open reduction with internal fixation is used, the affected limb should be elevated postoperatively. The degree of swelling, sensory and motor function, and blood circulation of the limb should be closely monitored to prevent compartment syndrome.
Finger flexion and extension exercises should begin two weeks postoperatively, along with wrist mobility exercises. Elbow and shoulder joint mobility exercises should start after four weeks. Once imaging confirms fracture healing at 8-10 weeks, forearm rotational exercises can be introduced.
Fractures of the proximal third of the ulna accompanied by radial head dislocation (Monteggia fracture) may result from direct dorsal trauma or indirect violence from falling on an outstretched hand. In closed reduction, the radial head should be reduced first to restore forearm length. Reduction of the radial head often facilitates successful reduction of the overlapping ulna. If closed reduction fails, malunion or non-union occurs, or there is neurovascular involvement, open reduction with internal fixation is performed.
Fractures of the distal third of the radius with dislocation of the ulnar head (Galeazzi fracture) may be caused by direct trauma or transmitted indirect force. Diagnosis is straightforward through clinical examination and X-ray imaging. Initial treatment typically involves closed reduction and plaster fixation. In cases of unsuccessful reduction, open reduction with internal fixation using plates is performed.