Etiology
This type of fracture is often caused by indirect trauma. When falling, with the elbow in a semi-flexed or extended position and the palm striking the ground, force is transmitted upward along the forearm. The body leans forward, generating shearing stress from above, which may cause a fracture at the junction between the humeral shaft and the humeral condyle. Typically, the proximal fragment displaces anteriorly and inferiorly, while the distal fragment displaces superiorly. If lateral force is applied during the fall, the fracture may also displace medially or laterally.
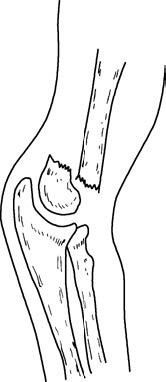
Figure 1 Typical displacement in extension-type supracondylar humeral fractures

Figure 2 Medial displacement of the distal fragment

Figure 3 Lateral displacement of the distal fragment
Clinical Presentation and Diagnosis
In children, a history of injury involving a fall onto an outstretched hand resulting in elbow pain, swelling, and subcutaneous bruising, with posterior protrusion of the elbow in a semi-flexed position, raises suspicion of a supracondylar humeral fracture. Examination may reveal localized tenderness, bone crepitus, and pseudo-joint motion, with the fracture fragment palpable at the anterior aspect of the elbow. The triangular relationship of the posterior elbow landmarks generally remains intact.
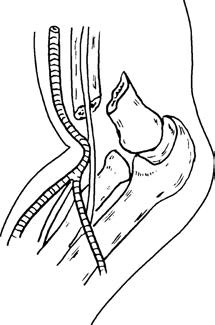
Figure 4 Anterior displacement of the proximal fragment compressing the brachial artery
Evaluation should carefully assess for neurovascular injury. Particular attention is required to observe the degree of forearm swelling, the presence of a radial pulse at the wrist, and sensation and motor function of the hand. Imaging with anteroposterior and lateral X-rays of the elbow is necessary, as it confirms the presence of a fracture, determines the displacement pattern, and provides critical information for treatment planning.
Treatment
Closed Reduction and External Fixation
For patients with a short duration of injury, minimal swelling, and no circulatory compromise, closed reduction and external fixation may be performed. Once X-ray imaging confirms good alignment of the fracture, external fixation can maintain reduction. Restoring the anterior tilt of the distal humerus and the carrying angle of the elbow is important. The degree of elbow flexion depends on the presence of a palpable radial pulse and the absence of sensory or motor deficits. Posterior splint immobilization in a flexed position for 4–5 weeks may be used, and once X-ray evaluation confirms satisfactory fracture healing, plaster can be removed, and functional exercises may begin. If closed reduction fails to achieve satisfactory alignment after 2–3 attempts, open reduction and internal fixation are recommended. In cases of prolonged injury duration, severe soft tissue damage, or significant swelling at the fracture site that contraindicates immediate closed reduction, open reduction and internal fixation should also be considered.
Surgical Treatment
Surgical treatment is recommended in the following cases:
- Failure of closed reduction.
- Presence of small open wounds with minimal contamination.
- Associated neurovascular injury.
Rehabilitation Therapy
Regardless of the treatment method, postoperative monitoring of limb circulation and sensory and motor function of the hand is essential. Elevating the affected limb and initiating early finger and wrist flexion and extension exercises help to alleviate swelling. Elbow flexion and extension exercises may begin 4–6 weeks after injury. For patients with stable open reduction and internal fixation, elbow joint mobilization can start as early as 2 weeks post-surgery.
In extension-type supracondylar humeral fractures, anterior and inferior displacement of the proximal fragment frequently compresses or punctures the brachial artery. Severe swelling due to tissue injury further compromises distal limb circulation and may result in forearm compartment syndrome. Failure to diagnose and manage the condition early can lead to ischemic contractures, significantly impacting hand function and limb development.
During the diagnosis and treatment of supracondylar humeral fractures, careful observation of forearm swelling and hand sensory and motor function is critical. Signs such as high-tension swelling, restricted active finger movements, severe pain during passive movements, a diminished or absent radial pulse, reduced skin temperature of the fingers, and sensory disturbances are indicative of elevated compartment pressure. Emergency surgical intervention is necessary to prevent ischemic contractures. Fasciotomy of the volar and dorsal compartments of the forearm can decompress the affected tissues. Additional treatments, such as dehydration therapy and vasodilator administration, may help prevent forearm ischemic contracture. If signs of the "5P" syndrome (painlessness, pulselessness, pallor, paresthesia, and paralysis) are present, treatment may be too late. Even with surgical decompression, ischemic contractures may be unavoidable.