Anatomical Overview
A humeral shaft fracture is defined as a fracture occurring between 1–2 cm distal to the surgical neck of the humerus and 2 cm proximal to the humeral condyles. The posterior lateral surface of the middle to distal third of the humeral shaft contains the radial groove, through which the radial nerve courses closely along the bone from the posteromedial to anterolateral direction before entering the forearm. Fractures in this region are prone to radial nerve injury, which may result from direct irritation by fracture fragments or compression by the lateral intermuscular septum.
Etiology and Classification
Humeral shaft fractures may arise from direct or indirect trauma. Direct trauma, such as a lateral blow to the midshaft, typically causes transverse or comminuted fractures. Indirect trauma, such as falling onto an outstretched hand or elbow, transmits force upward along the humerus, combined with shearing stress from body weight, leading to fractures in the middle to distal third. Spiral or oblique fractures of the middle to distal third may also occur during forceful throwing or arm wrestling.
Fracture displacement depends on the magnitude and direction of the applied force, fracture location, and muscular traction. Specific patterns include:
- Fractures proximal to the deltoid insertion but distal to the pectoralis major insertion: The proximal fragment is pulled medially and anteriorly by the pectoralis major, latissimus dorsi, and teres major muscles, while the distal fragment shifts laterally and proximally due to traction from the deltoid, coracobrachialis, biceps brachii, and triceps brachii.
- Fractures distal to the deltoid insertion: The proximal fragment displaces anteriorly and laterally by the deltoid muscle, while the distal fragment is drawn proximally by the biceps and triceps brachii.
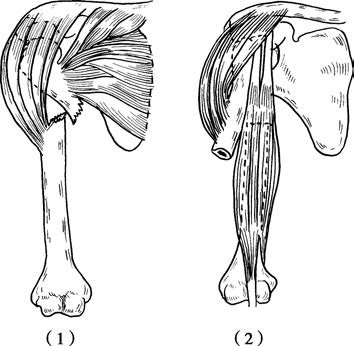
Figure 1 Displacement in humeral shaft fractures
(1) Fracture located above the deltoid insertion.
(2) Fracture located below the deltoid insertion.
Regardless of the fracture level, gravitational forces from the limb or improper external fixation may cause separation, rotational malalignment, or angulation. Fractures in the distal third of the humeral shaft often exhibit angulation, shortening, and rotational deformities influenced by the direction of trauma and the position of the forearm and elbow.
Clinical Presentation and Diagnosis
Following injury, pain, swelling, deformity, subcutaneous bruising, and restricted mobility of the upper limb may occur in the upper arm. Examination may reveal pseudo-joint motion, bone crepitus, and diminished or absent bone conduction sounds. X-rays can confirm the type of fracture and the direction of displacement.
Radial nerve damage, if present, may result in wrist drop, an inability to extend the metacarpophalangeal joints of the fingers and the thumb, difficulty in forearm supination, and reduced or absent sensation on the radial side of the dorsum of the hand.
Treatment
Humeral shaft fractures of transverse or short oblique types can be managed with either non-surgical or surgical methods.
Closed Reduction and External Fixation
Fracture reduction is performed under adequate continuous traction and muscle relaxation. The surgeon uses both hands to realign the fracture ends by counteracting the displacement, correcting the angular deformity and lateral displacement. X-rays are performed on all patients after reduction to confirm proper alignment and apposition of the fracture. Once reduction is successful, traction can be reduced to maintain the alignment. A plaster cast is an option for immobilization, with stringent monitoring of fracture alignment during the fixation period.
Open Reduction and Internal Fixation
Indications for surgery include:
- Failure of closed reduction leading to poor alignment and apposition, potentially impairing function after healing.
- Presence of separated displacement or soft tissue entrapment at the fracture site.
- Associated neurovascular injuries.
- Nonunion of chronic fractures.
- Malunion causing functional impairment.
- Multiple fractures within the same limb.
- Open fractures with mild contamination within 8–12 hours post-injury.
Surgical Approach
Under anesthesia, the surgical approach is chosen based on the fracture type, its location, and the surgeon's experience. Care is taken to avoid damage to the radial nerve during the procedure. Anatomical alignment is achieved under direct visualization whenever possible. Early functional exercises are initiated postoperatively. Fractures in the distal third of the humeral shaft disrupt blood supply significantly, and surgical manipulation can further hinder healing. Recently, minimally invasive surgical techniques have been employed to minimize disruption to blood flow, promoting fracture healing.
For patients with radial nerve injury, intraoperative exploration of the nerve may be undertaken. If a complete transection is detected, primary repair of the radial nerve can be performed. For cases of nerve contusion where continuity remains intact, the epineurium may be incised to mitigate secondary pathological changes.
Rehabilitation Therapy
Regardless of whether closed reduction with external fixation or open reduction with internal fixation is chosen, early rehabilitation therapy is emphasized postoperatively. The affected limb can be elevated after reduction, followed by active finger flexion and extension exercises. Two to three weeks later, active extension and flexion exercises of the wrist and elbow joints, along with abduction and adduction of the shoulder joint, may begin. After six to eight weeks, the intensity of exercises can be increased, introducing shoulder joint rotation motions. Regular monitoring of fracture alignment and healing status is recommended.