Anatomical Overview
The joints involved in shoulder movement include the glenohumeral joint, acromioclavicular (AC) joint, sternoclavicular joint, and scapulothoracic joint (formed by the scapula and the thoracic wall). Among these, the glenohumeral joint plays the most significant role in movement. The dislocation of the glenohumeral joint is commonly referred to as a shoulder joint dislocation.
The glenohumeral joint is formed by the humeral head and the glenoid cavity of the scapula. The glenoid cavity is shallow and is deepened by the surrounding fibrocartilage and the glenoid labrum. Additionally, the acromion forms a socket-like structure above the humeral head and glenoid cavity (sometimes referred to as a second joint), which provides some degree of stability while allowing a wide range of shoulder movement.
Etiology and Classification
Trauma serves as the primary cause of shoulder joint dislocation, often resulting from indirect forces. When falling or experiencing an impact, the force is transmitted through the upper limb to the shoulder joint, causing the humeral head to breach the joint capsule and become dislocated. Direct impact of the humeral head against a hard object may also result in dislocation.
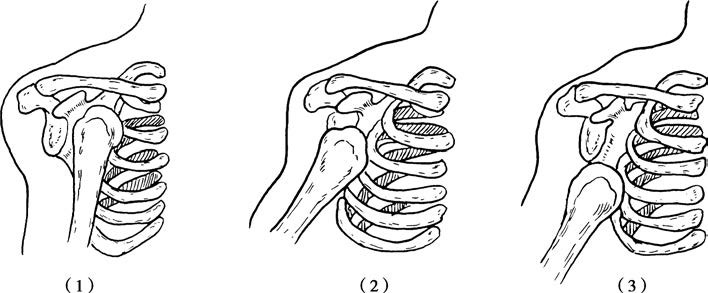
Figure 1 Classification of three types of shoulder dislocations
(1) Subclavicular Dislocation, (2) Subcoracoid Dislocation, (3) Infraglenoid Dislocation
Based on the direction of humeral head displacement, shoulder dislocations can be classified into anterior, posterior, superior, and inferior types, with anterior dislocations being the most common. Depending on the magnitude and direction of the force, as well as muscle tension, anterior dislocations may position the humeral head beneath the clavicle, below the coracoid process, anterior to the shoulder, or beneath the glenoid cavity.
Clinical Manifestations and Diagnosis
A history of injury involving landing on an outstretched upper limb, accompanied by shoulder pain, swelling, and impaired shoulder joint movement, should raise suspicion of a shoulder dislocation. Patients often exhibit a characteristic posture, using the uninjured hand to support the forearm of the affected side, with the head tilted toward the injured shoulder. Examination may reveal a squared shoulder deformity, a hollow sensation at the glenoid cavity, and elastic fixation of the upper limb.
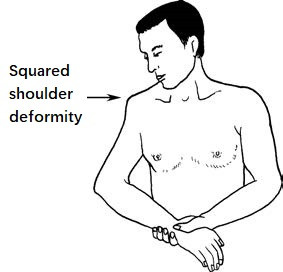
Figure 2 Squared shoulder deformity associated with anterior shoulder dislocation
A positive Dugas sign can be observed, where the patient is unable to touch the opposite shoulder with the affected side’s palm while keeping the elbow close to the chest, or cannot bring the elbow close to the chest while placing the palm on the opposite shoulder. X-ray images, including anteroposterior, lateral, and axial views, can confirm the type and direction of the dislocation, as well as the presence of associated fractures. CT scans are now routinely used in clinical practice to assess shoulder dislocations.
In cases of severe trauma, anterior shoulder dislocations may be associated with neurovascular injuries in the affected upper limb. Sensory and motor function of the affected limb should be carefully examined.
Treatment
Anterior shoulder dislocations are primarily treated with closed reduction under anesthesia and external fixation. Posterior dislocations may be more challenging to treat with closed reduction alone and often require open reduction combined with external fixation. It is crucial to accurately identify any fractures before attempting reduction to avoid misdiagnosis.
Closed Reduction Technique
The Hippocrates method is commonly employed for reduction. The patient lies supine while the practitioner stands on the side of the affected shoulder. A cotton pad is placed in the axilla for cushioning, and the practitioner positions their ipsilateral heel under the patient’s axilla against the chest wall. The practitioner grips the affected limb, abducts it, and applies gentle traction, using the heel to provide countertraction. For a left shoulder dislocation, the practitioner uses their left foot, while the right foot is used for right shoulder dislocations. Sustained and even traction is necessary until the shoulder muscles relax. At this point, the arm is adducted and internally rotated, allowing the humeral head to slide through the anterior tear in the capsule and return to the glenoid cavity, often accompanied by a noticeable click or springy sensation, indicating successful reduction. A Dugas test performed afterward should turn negative.
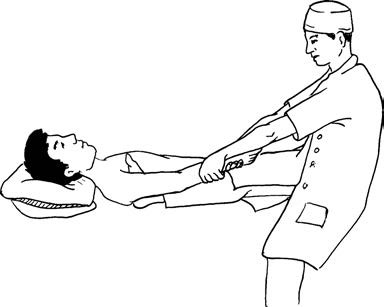
Figure 3 Hippocrates method for reducing anterior shoulder dislocations
Fixation Methods
For simple shoulder dislocations, after reduction, the upper limb can be suspended in a triangular sling with the elbow flexed to 90 degrees, and a cotton pad placed under the axilla for support, typically for three weeks. If a displaced fracture of the greater tuberosity is present, the fixation period may be extended by 1 to 2 weeks.
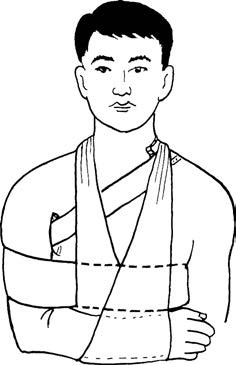
Figure 4 External fixation following shoulder reduction
In some cases, significant capsule damage or insufficient strength of the shoulder girdle muscles may lead to subluxation, even after treatment. For such cases, a chest-humerus bandage in the “shoulder-clasping position” is recommended. This involves placing the affected hand on the opposite shoulder with the elbow close to the chest, securing the upper arm to the chest with a bandage while supporting the elbow. This position helps correct subluxation of the shoulder joint.
Rehabilitation
During the fixation period, wrist and finger movements should be maintained. Following the removal of fixation, patients are encouraged to perform active exercises to restore movement in all directions of the shoulder joint. Physical therapy and massage may enhance recovery. Rehabilitation should be gradual and cautious to avoid complications.
For chronic shoulder dislocations that impair upper limb function, surgical open reduction can be considered to repair the joint capsule and ligaments. In cases of nerve damage, most patients experience some degree of neural recovery following reduction. However, if nerve or vascular rupture is suspected, timely surgical repair is necessary.