Anatomical Overview
The acromioclavicular (AC) joint is formed by the articulation between the clavicular facet of the acromion and the acromial facet of the lateral clavicle. Some joints contain a fibrocartilaginous disc within the articular space. The joint surfaces are typically oriented vertically, and the joint capsule is thin, with stability primarily maintained by surrounding ligaments. The key stabilizing ligaments are the acromioclavicular ligament and the coracoclavicular ligament.
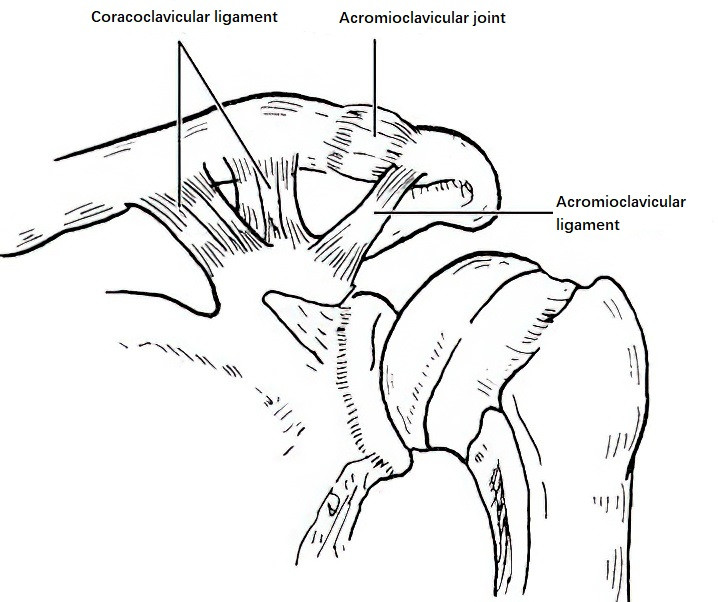
Figure 1 Anatomical structures of the acromioclavicular joint
Etiology and Classification
Acromioclavicular joint dislocation is common, particularly among young adults, and is primarily caused by trauma, with direct trauma being more frequent. A direct blow to the acromion drives the acromion and scapula downward, resulting in rupture of the joint capsule and ligaments. Indirect trauma, such as falling onto the shoulder with force transmitted to the AC joint, may also cause dislocation. Depending on the severity of the trauma, injuries may range from contusion or partial tearing of the joint capsule and ligaments to complete ligament rupture, avulsion fractures, subluxation, or complete dislocation. AC joint dislocations are classified into three types based on severity:
- Type I: Contusion of the AC joint capsule and ligaments without rupture.
- Type II: Rupture of the AC joint capsule with partial ligament injury or tearing, leading to subluxation.
- Type III: Complete rupture of the AC joint capsule and ligaments, resulting in full dislocation.
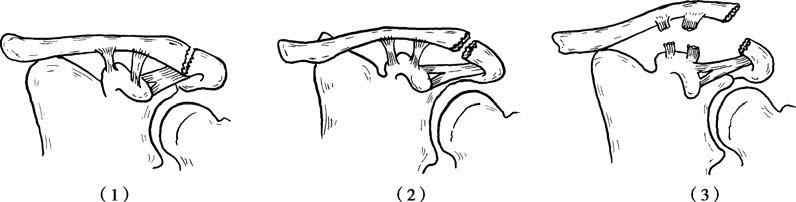
Figure 2 Classification of acromioclavicular joint dislocations
Clinical Presentation and Diagnosis
Type I
A history of shoulder trauma is present, with pain and swelling at the acromioclavicular (AC) joint. Pain worsens during movement, and there is significant localized tenderness. X-rays of the shoulder or clavicle show no obvious displacement.
Type II
In addition to the clinical manifestations and signs of Type I, there is a palpable "springiness" when pressing on the distal end of the clavicle. X-rays reveal an upward elevation of the distal clavicle, indicating partial dislocation.
Type III
In addition to the clinical manifestations and signs of Type I, there is significant swelling above the outer shoulder. A comparison with the contralateral side shows a noticeable protrusion on the affected side. Increased "springiness" is observed upon palpation, and shoulder joint movement is restricted. X-rays show a complete dislocation where the joint surfaces of the distal clavicle and acromion are entirely misaligned.
Treatment
Type I
The affected limb is supported with a triangular bandage for 2–3 weeks, followed by gradual shoulder mobilization, which typically yields good functional recovery.
Type II
Closed reduction with padded external fixation may be attempted, but fixation is often unreliable and carries risks of pressure ulcers or chronic subluxation.
Type III and Symptomatic Chronic Subluxations
Surgical intervention is recommended, especially for dislocations with over 2 cm of displacement. Surgical options include open reduction with internal fixation (e.g., tension band fixation). If the coracoclavicular ligament is irreparable, ligament reconstruction or stabilization may be performed. Concurrent repair of ruptured ligaments (e.g., AC or coracoclavicular ligaments) is often attempted during surgery.

Figure 3 Tension band fixation for acromioclavicular joint dislocation