In certain complex injuries, the fracture itself may not be the primary concern; the associated or resulting damage to critical tissues or organs can have more significant consequences, often triggering severe systemic reactions and, in some cases, posing a life-threatening risk. Complications that arise during fracture management can seriously impact treatment outcomes and require careful prevention and timely, appropriate intervention.
Early Complications
Shock
Shock can result from severe trauma, massive hemorrhage caused by fractures, or damage to vital organs.
Fat Embolism Syndrome (FES)
Fat embolism syndrome typically occurs in adults, especially young and middle-aged individuals with femoral shaft fractures. It is caused by excessive hematoma tension within the medullary cavity and bone marrow destruction, allowing fat droplets to enter ruptured venous sinuses, leading to pulmonary and cerebral fat embolism. Clinically, it manifests as hypoxemia, neurological abnormalities, and petechial rash.
Injuries to Vital Organs
Liver and Spleen Rupture
Severe injuries to the lower chest wall, in addition to causing rib fractures, may also result in rupture and hemorrhage of the spleen on the left side or the liver on the right side, potentially leading to shock.
Lung Injuries
Rib fractures can damage intercostal blood vessels and lung tissue at the fracture site, causing conditions such as pneumothorax, hemothorax, or hemopneumothorax, which may lead to severe respiratory distress.
Bladder and Urethral Injuries
Commonly associated with pelvic fractures, these injuries may cause urine leakage, resulting in pain, swelling, and bruising in the lower abdomen and perineal region, as well as hematuria and difficulty urinating.
Rectal Injuries
Sacrococcygeal fractures can cause rectal injuries, leading to lower abdominal pain and rectal bleeding.
Injuries to Surrounding Tissues
Damage to Major Blood Vessels
This is commonly seen in fractures such as supracondylar fractures of the femur, where the distal fracture end may injure the popliteal artery; proximal tibial fractures, which may harm the anterior or posterior tibial artery; and extension-type supracondylar fractures of the humerus, where the proximal fracture end can easily damage the brachial artery.
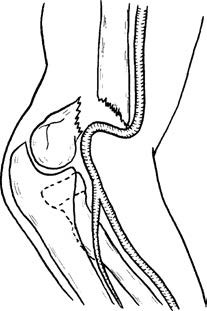
Figure 1 Brachial artery injury resulting from extension-type supracondylar fracture of the humerus.
Injury to Surrounding Nerves
Nerve injuries are especially likely in areas where nerves are closely adjacent to bones. For instance, fractures at the junction of the middle and lower thirds of the humerus can easily damage the radial nerve that runs along the radial groove of the humerus.
Spinal Cord Injuries
Spinal fractures and dislocations may lead to serious spinal cord injuries, particularly in the cervical and thoracolumbar regions. Such injuries can result in paralysis below the level of the neurological injury.
Osteofascial Compartment Syndrome (OCS)
Osteofascial compartment syndrome is an acute syndrome characterized by ischemia of muscles and nerves within a compartment formed by bone, interosseous membranes, fascial septa, and deep fascia. It is commonly seen on the palmar side of the forearm or in the lower leg. This condition often arises from hematoma formation and tissue swelling following traumatic fractures, which increase the volume of the compartment’s contents. It may also be caused by excessively tight external bandages or local compression that reduces the compartment volume, leading to increased intracompartmental pressure. When the intracompartmental pressure reaches a critical level, the small arteries supplying the muscles may close, initiating a vicious cycle of ischemia–edema–ischemia. Depending on the degree of ischemia, potential outcomes include:
Impending Ischemic Contracture
In the early stages of ischemia, timely management to restore blood supply can prevent muscle necrosis or result in only minimal necrosis without functional impairment of the limb.
Ischemic Contracture
In cases of short-term or more severe incomplete ischemia, significant muscle necrosis occurs even after blood supply is restored, leading to contracture deformities (e.g., Volkmann’s ischemic contracture), which severely impact limb function.
Gangrene
Prolonged and extensive complete ischemia causes massive muscle necrosis (gangrene), often necessitating amputation. The release of large amounts of toxins into the bloodstream may lead to complications such as shock, arrhythmias, and acute renal failure.
Early diagnosis of osteofascial compartment syndrome can be made based on the following four signs:
- Sensory abnormalities in the affected limb.
- Pain during passive stretching of the involved muscles (positive passive stretch test).
- Pain during active flexion of the muscles.
- Tenderness over the muscle belly within the compartment.
Osteofascial compartment syndrome may also lead to complications such as myoglobinuria and hyperkalemia. Treatment requires sufficient fluid resuscitation to promote diuresis. If the compartment pressure exceeds 30 mmHg or the pressure gradient (diastolic pressure minus compartment pressure) falls below 30 mmHg, fasciotomy should be performed promptly to relieve pressure.
Late Complications
Hypostatic Pneumonia
Hypostatic pneumonia primarily occurs in patients who are bedridden for extended periods due to fractures, especially elderly, debilitated individuals or those with chronic illnesses. It can occasionally become life-threatening.
Decubitus Ulcers
Decubitus ulcers may develop in patients with severe traumatic fractures who remain bedridden for extended periods. Prolonged pressure on bony prominences can lead to local blood circulation impairment and ulcer formation. Common sites include the sacrum, hips, and heels. Paraplegic patients, due to the loss of nerve innervation and lack of sensation, are particularly prone to decubitus ulcers. Poor local circulation not only makes these ulcers more likely to occur but also renders them difficult to heal, often becoming a source of systemic infection.
Deep Vein Thrombosis (DVT)
Deep vein thrombosis is commonly observed in cases of pelvic fractures or lower limb fractures. Prolonged immobilization of the lower extremities, combined with trauma-induced hypercoagulable states, can lead to venous thrombosis.
Infection
Infection rates range from 1% to 5%. Factors such as poor local blood supply to the fracture site, impaired soft tissue integrity, incomplete debridement of open fractures, or inadequate soft tissue coverage can contribute to infections, which may progress to suppurative osteomyelitis.
Traumatic Myositis Ossificans
Traumatic myositis ossificans, also known as heterotopic ossification, occurs around joints due to sprains, dislocations, or fractures near a joint. When subperiosteal hematoma forms because of periosteal stripping and is improperly managed, the hematoma may enlarge, undergo organization, and lead to extensive ossification within the soft tissue around the joint. Severe cases result in significant joint movement dysfunction. This condition is most commonly observed around the elbow joint.
Traumatic Arthritis
Traumatic arthritis often results from intra-articular fractures that fail to achieve anatomical reduction. Irregularities in the joint surface after bone healing can cause persistent joint pain during movement due to chronic wear and tear.
Joint Stiffness
Prolonged immobilization of the affected limb can lead to venous and lymphatic drainage issues. Serofibrinous exudation and fibrin deposition within the perijoint tissues may cause fibrous adhesions. Concurrently, contractures of the joint capsule and surrounding muscles can result in restricted joint mobility.
Acute Bone Atrophy (Sudeck's Atrophy)
Acute bone atrophy, also known as reflex sympathetic dystrophy, is characterized by painful osteoporosis and soft tissue atrophy near the joint due to injury. It frequently occurs after fractures of the hands or feet. Typical symptoms include pain and vascular dysregulation. The intensity of the pain is disproportionate to the severity of the injury and worsens with movement of nearby joints. A burning sensation is often present. Muscle spasm around the joint leads to joint stiffness. Vascular dysregulation initially manifests as elevated skin temperature, edema, and accelerated growth of hair and nails. Over time, skin temperature drops, excessive sweating occurs, the skin becomes smooth, and hair loss is noted. Swelling, stiffness, coldness, and a slightly cyanotic appearance of the hand or foot can persist for several months.
Avascular Osteonecrosis
Avascular osteonecrosis can occur when the blood supply to a fracture fragment is disrupted, leading to ischemic necrosis of the affected bone. Common examples include avascular necrosis of the proximal scaphoid following scaphoid fractures and femoral head necrosis after femoral neck fractures.

Figure 2 Avascular necrosis of the femoral head after femoral neck fracture.
(1) Diagram of femoral neck blood supply and fracture.
(2) Secondary femoral head avascular necrosis resulting from femoral neck fracture.
Ischemic Contracture
Ischemic contracture is one of the most severe complications of fractures and represents the serious consequences of inadequately managed osteofascial compartment syndrome. It can be directly caused by fractures and associated soft tissue injuries, but more commonly, improper handling of fractures such as overly tight external fixation contributes to the condition. Recognizing osteofascial compartment syndrome early and managing it appropriately is vital for preventing ischemic contracture. Once it occurs, treatment becomes extremely challenging with poor outcomes, often resulting in significant disability. A typical deformity associated with ischemic contracture is claw hand or claw foot.
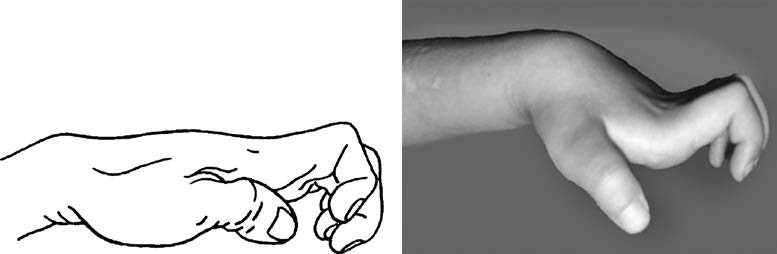
Figure 3 Typical deformity of claw hand following ischemic contracture of the forearm.