Scoliosis refers to a spinal deformity in which one or more segments of the spine curve laterally, often accompanied by vertebral rotation. According to the Scoliosis Research Society, scoliosis is defined when the lateral curvature of the spine exceeds 10° as measured by the Cobb method on a standing anteroposterior X-ray.
Classification
Scoliosis is broadly divided into two categories: non-structural scoliosis and structural scoliosis.
Non-structural Scoliosis
Non-structural scoliosis does not involve intrinsic changes to the spine or its supporting structures. The deformity can be corrected in lateral bending or through treatment of the underlying cause, and the scoliosis resolves. Potential causes of non-structural scoliosis include:
- Postural scoliosis
- Hysterical scoliosis
- Irritation of nerve roots, such as in cases of intervertebral disc herniation or tumors
- Inflammatory conditions
- Leg length discrepancies
- Hip joint contractures
Structural Scoliosis
Structural scoliosis involves a fixed lateral curvature and vertebral rotation that cannot be corrected through postural adjustments or lateral bending. Even when initially corrected, it cannot be maintained due to fixation of the affected vertebrae in a rotated position. Structural scoliosis can be further classified based on the underlying cause:
- Idiopathic scoliosis
- Congenital scoliosis
- Neuromuscular scoliosis
- Scoliosis associated with neurofibromatosis
- Scoliosis associated with mesenchymal abnormalities
- Scoliosis associated with osteochondrodysplasia
- Scoliosis associated with metabolic disorders
- Scoliosis resulting from other causes
Idiopathic Scoliosis (IS)
This is the most common type of scoliosis, accounting for approximately 75–80% of all cases, with an unknown etiology. It commonly occurs in adolescents and is more frequent in females. Idiopathic scoliosis is classified by age of onset:
- Infantile type (0–3 years)
- Juvenile type (4–10 years)
- Adolescent type (11–18 years)
- Adult type (>18 years)
Congenital Scoliosis
This type arises from spinal developmental abnormalities and is further subdivided into three categories based on the nature of the anomaly:
- Formation defects: Examples include hemivertebrae and wedge-shaped vertebrae.
- Segmentation defects: Includes unilateral unsegmented bony bridges and bilateral unsegmented vertebrae (block vertebrae).
- Mixed type: A combination of formation defects and segmentation defects.
Pathology
Despite differing etiologies, the pathological changes associated with various forms of scoliosis are similar.
Changes in Spinal Structure
The vertebral bodies on the concave side of the curvature become wedge-shaped and rotate. In the primary curve, the vertebral bodies rotate toward the convex side, while the spinous processes rotate toward the concave side. The pedicles on the concave side become shorter and narrower, and the laminae on the concave side are slightly smaller compared to the convex side. Tilting of the spinous processes narrows the spinal canal on the concave side. The facet joints on the concave side thicken and undergo sclerosis, forming bony spurs.
Changes in Discs, Muscles, and Ligaments
The intervertebral spaces narrow on the concave side and widen on the convex side. Muscles on the concave side may exhibit slight contractures.
Changes in Ribs
As the vertebrae rotate, the ribs on the convex side shift posteriorly, causing a posterior thoracic prominence (rib hump), and in severe cases, this leads to a "razor-back" deformity. The ribs on the convex side separate from each other, increasing intercostal spaces, while the ribs on the concave side are compressed and move anteriorly, resulting in chest wall asymmetry.
Changes in Internal Organs
Severe thoracic deformities can cause compression and alterations in the shape of the lungs, potentially leading to pulmonary heart disease in extreme cases.
Clinical Manifestations
In the early stages, the deformity is often subtle and may go unnoticed. During periods of rapid growth, such as adolescence, scoliosis progresses rapidly. Height may lag behind that of peers, and there may be asymmetry in shoulder height or the thoracic cage. Severe scoliosis can result in a "razor-back" appearance, compromise cardiopulmonary function, or produce symptoms related to neural tension or compression.
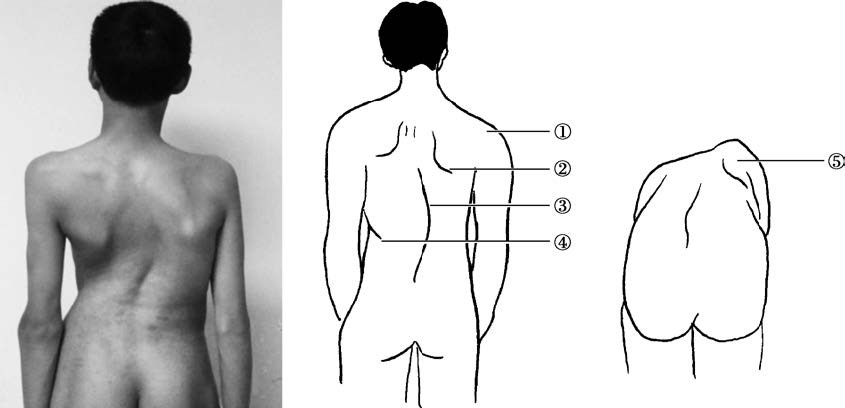
Figure 1 Appearance of scoliosis
1, Unequal shoulder heights
2, Unequal scapular heights
3, Spine deviation from the midline
4, Waist asymmetry with skin folds on one side
5, Asymmetry of the back during forward bending, forming a "razor-back" appearance
Physical Examination
Examination should include adequate exposure of the patient. The examiner should observe the patient from the front, back, and sides, noting any abnormalities. Observation includes checking for skin changes such as pigmentation, subcutaneous masses, abnormal hair growth, or cystic formations. Attention is paid to breast development and symmetry of the thoracic cage.
Forward bending tests are conducted to assess for rib or spinal prominence due to rotation, as indicated by asymmetry. Shoulder level symmetry is observed. A plumb line can be dropped from the C7 spinous process to measure the distance from the gluteal cleft, assessing for trunk imbalance. Spinal range of motion and neurological status are also evaluated. Height and weight are documented.
Ancillary Examinations
X-Ray Examinations
Standing Full-Length Anteroposterior and Lateral X-Ray Views
These serve as the fundamental diagnostic tools for scoliosis. The patient must remain in a standing position during imaging, as lying down causes muscle relaxation that can reduce the apparent degree of curvature. The imaging range should encompass the entire spine.

Figure 2 Standing full-length anteroposterior spinal X-ray
Bending, Traction, and Fulcrum Views
Supine maximum left- and right-side bending (bending views), gravity traction (traction views), and fulcrum-bending views allow for an understanding of spinal flexibility. These views are invaluable for guiding treatment decisions.
Derotational (Stagnara) Views
For cases of severe scoliosis, particularly when accompanied by kyphosis or significant vertebral rotation, standard X-rays may not adequately display abnormalities in ribs, transverse processes, or vertebral bodies. Derotational views provide a clearer depiction of these structures and help assess the vertebral deformities comprehensively.
Scoliosis X-Ray Measurements
Cobb Method
This is the most commonly used method. The Cobb angle is determined by the intersection of perpendicular lines from the upper endplate of the uppermost vertebra and the lower endplate of the lowermost vertebra of the curve.
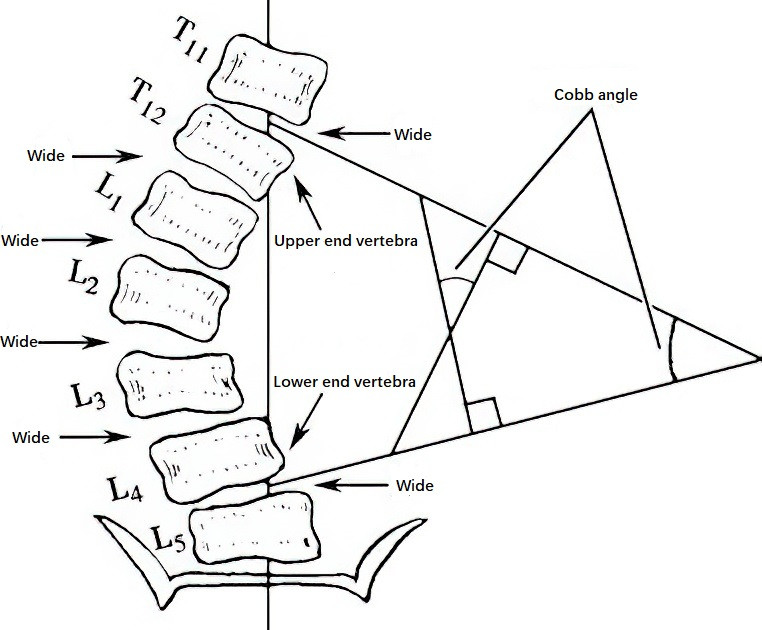
Figure 3 Cobb method for scoliosis X-ray measurement
Ferguson Method
This is rarely used and is mainly applicable for mild scoliosis (<50°). It calculates the angle between lines connecting the center of the apical vertebra to the centers of the upper and lower end vertebrae.
Measurement of Vertebral Rotation
This is commonly performed using the Nash-Moe method, which grades rotation into 5 levels based on the position of the pedicles on an anteroposterior X-ray:
- Grade 0: Pedicles are symmetric.
- Grade I: The pedicle on the convex side shifts toward the midline but does not surpass the first quarter; the pedicle on the concave side appears smaller.
- Grade II: The pedicle on the convex side shifts to the second quarter, and the pedicle on the concave side disappears.
- Grade III: The pedicle on the convex side reaches the midline, while the pedicle on the concave side disappears.
- Grade IV: The pedicle on the convex side crosses the midline and approaches the concave side.
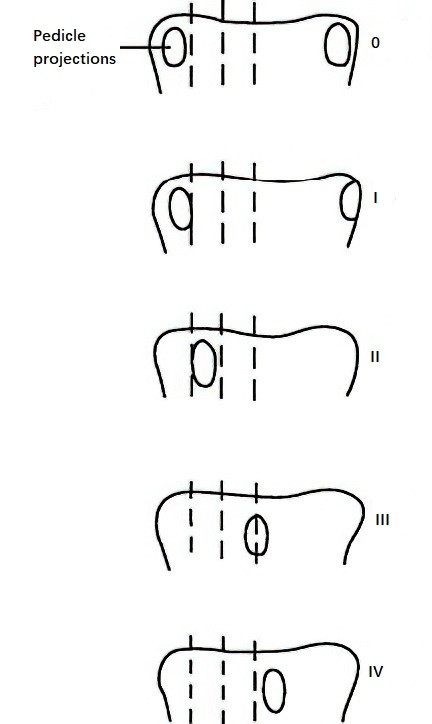
Figure 4 Vertebral rotation measurement method
Additional Imaging Studies
CT (Computed Tomography)
CT scans are particularly beneficial for diagnosing abnormalities in the spine, spinal cord, and nerve roots. They are especially advantageous for areas that are poorly visualized on standard X-rays (e.g., craniocervical or cervicothoracic junction). CT clearly displays the fine structures of vertebrae, the spinal canal, and paraspinal tissues. CT myelography (CTM) can provide insights into the spinal canal's condition and the relationship between bone, the spinal cord, and nerves, offering essential information for surgical planning. In recent years, 3D reconstruction of spinal CT has enhanced the visualization of deformities and provides critical imaging data for screw placement and osteotomy during surgery.
MRI (Magnetic Resonance Imaging)
MRI is highly effective for detecting intraspinal abnormalities. It offers superior resolution for assessing lesion location, extent, and characteristics, such as edema, compression, hematoma, spinal cord malformation, or degeneration. However, its visualization of bony structures is comparatively inferior to CT.
Myelography
In cases of scoliosis, it is essential to evaluate not only vertebral and spinal abnormalities but also any associated intraspinal malformations. Myelography is useful for identifying neurological abnormalities that coexist with skeletal deformities.
Pulmonary Function Testing
Pulmonary function testing is a routine evaluation for patients with scoliosis. Total lung capacity (TLC) and vital capacity (VC) are reduced, while residual volume often remains normal. The degree of vital capacity reduction correlates with the severity of the scoliosis.
Electrophysiological Examination
Electrophysiological studies provide critical insights into whether scoliosis is accompanied by neurological or muscular system abnormalities.
Electromyography (EMG)
EMG assesses the status of motor units and evaluates the function of nerves and muscles.
Nerve Conduction Velocity (NCV)
NCV measures both motor conduction velocity and sensory conduction velocity. Multiple factors influence conduction velocity; for unilateral lesions, the contralateral side should serve as a comparison.
Evoked Potentials
Somatosensory evoked potentials (SEP) assess sensory function and help determine the extent of spinal cord and nerve injury. They are useful for evaluating treatment outcomes and monitoring progress.
Intraoperative Spinal Cord Monitoring
Intraoperative spinal cord monitoring provides accurate and reliable information, ensuring patient safety during surgery and helping to prevent neurological injury. It significantly improves surgical outcomes. The primary spinal cord monitoring techniques include:
- Somatosensory evoked potentials (SEP)
- Motor evoked potentials (MEP)
- Electromyographic (EMG) monitoring of muscles innervated by specific spinal nerves
Assessment of Skeletal Maturity
Evaluating skeletal maturity is crucial in scoliosis management. Physiological age, chronological age, and bone age are used to assess the patient's skeletal maturity. The evaluation includes:
Secondary Sexual Characteristics
These include signs such as voice changes in boys, the onset of menstruation, and breast and pubic hair development in girls.
Bone Age
Wrist Bone Age
X-rays of the wrist can help determine bone age in patients under 20 years.
Risser Sign
This evaluates the progression of the iliac apophysis ossification from the anterior superior iliac spine to the posterior superior iliac spine, dividing its total length into four equal parts.
- Score 0: No ossification seen.
- Score I: Ossification in 1/4.
- Score II: Ossification in 2/4.
- Score III: Ossification in 3/4.
- Score IV: Complete ossification.
- Score V: Fusion of the iliac apophysis with the iliac crest.
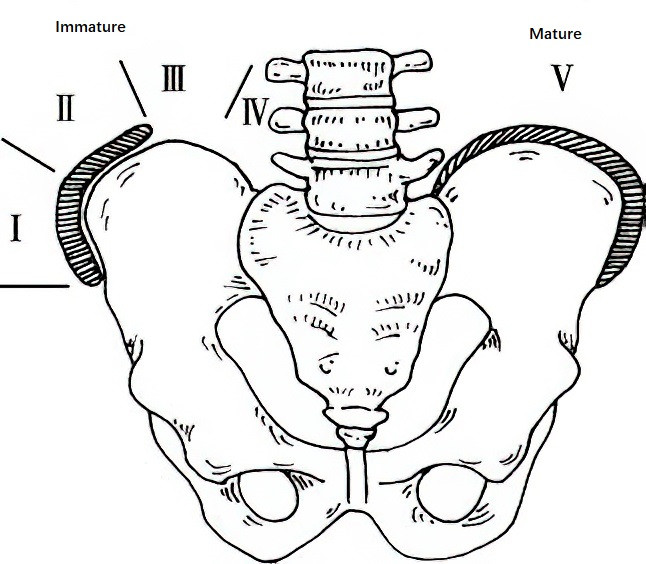
Figure 5 Risser sign measurement
Vertebral Endplate Epiphysis
Fusion of the epiphyseal ring with the vertebral body, seen on lateral X-rays, is an important indicator that spinal growth has ceased (skeletal maturity).
Y-Shaped Cartilage of the Acetabulum
Closure of the Y-shaped cartilage of the acetabulum indicates that spinal growth is nearing completion.
Treatment
The objectives of scoliosis treatment include the following:
- Correction of the deformity
- Achieving spinal stability
- Maintaining balance
- Slowing down or halting progression
Treatment principles and methods vary depending on the type of scoliosis. The following describes treatment strategies for adolescent idiopathic scoliosis as an example, including observation and follow-up, bracing, and surgical intervention.
Non-Surgical Treatment
Observation and Follow-Up
This approach is suitable for patients with a curvature of less than 20°. The primary goal is to monitor the progression of the spinal deformity. Follow-up evaluations are performed every 4 to 6 months, including routine standing full-length anteroposterior and lateral spinal X-rays.
Bracing
Bracing is the only effective non-surgical treatment for progressive idiopathic scoliosis. It is indicated for children in the growth phase with flexible curves between 20° and 40°. Braces are custom-made based on the patient's body size. Daily use of the brace for 16 to 23 hours is required until the skeletal structure reaches maturity. Standing full-length spinal X-rays are taken regularly, and braces are adjusted or replaced as needed. For girls, brace use generally continues until two years after menarche and Risser stage IV is reached. For boys, brace use typically continues until Risser stage V is reached. Brace treatment can then be gradually discontinued, with follow-up continuing for several years. If the brace fails to control progression and the Cobb angle continues to increase, surgical intervention becomes necessary.
Surgical Treatment
Severe or progressive scoliosis often requires surgical treatment. Indications for surgical intervention include:
- Ineffectiveness of bracing treatment
- Progressive scoliosis in children during the growth phase
- Imbalance of the spine
- Significant cosmetic deformity
Surgical treatment consists primarily of scoliosis correction and spinal fusion. Correction techniques are classified into anterior and posterior approaches, with some cases requiring a combination of both approaches. The primary goal of spinal fusion is to maintain the correction and ensure spinal stability.
Advancements in imaging techniques, materials science, and anatomy have significantly improved scoliosis surgery in various aspects, including classification, pedicle screw techniques, non-fusion technologies, spinal osteotomy techniques, and minimally invasive thoracoscopic techniques. The correction of scoliosis has advanced to a new level involving three-dimensional correction and three-dimensional stabilization.