Flat foot, also known as pes planus, refers to a congenital or postural condition characterized by a low or absent arch of the foot, resulting in valgus deformity of the affected foot. Arch collapse occurs during standing or walking, leading to symptoms such as fatigue or pain. It is generally categorized into postural flat foot (flexible flat foot) and rigid flat foot.
Applied Anatomy
The foot consists of 7 tarsal bones, 5 metatarsal bones, and 14 phalanges, forming longitudinal and transverse arches. The longitudinal arch is divided into two parts: medial and lateral.
The medial longitudinal arch is formed by the calcaneus, talus, navicular bone, first, second, and third cuneiform bones, and the first, second, and third metatarsal bones. This arch is higher and more mobile.
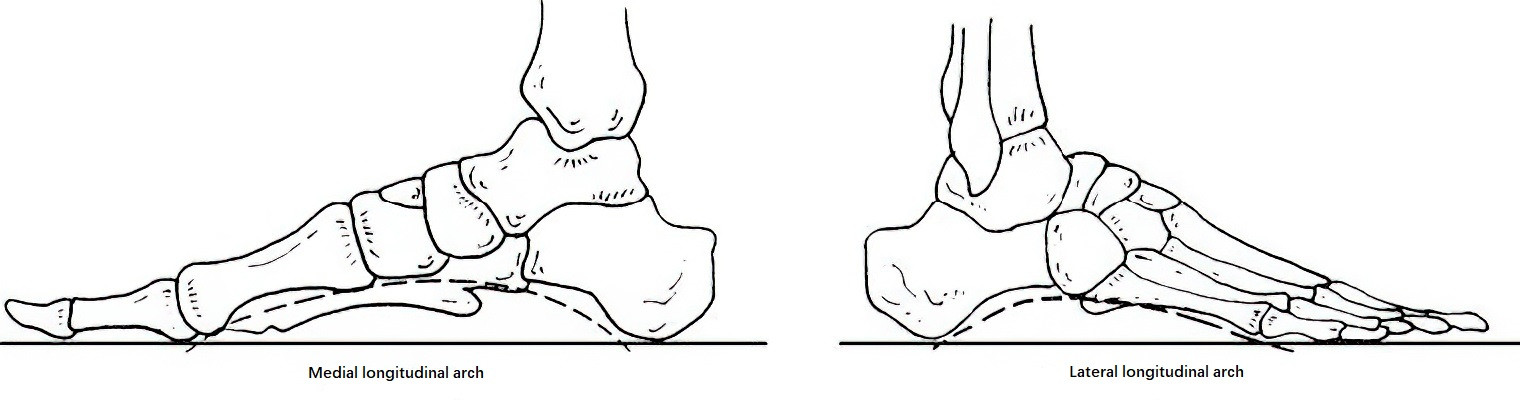
Figure 1 Longitudinal arches of the foot
The lateral longitudinal arch consists of the calcaneus, cuboid bone, and the lateral two metatarsal bones. This arch is relatively lower and disappears under weight-bearing, making the lateral foot the main load-bearing region.
The transverse arch is formed by the cuboid bone, three cuneiform bones, and the bases of the metatarsals. The highest point is located at the cuneiform-cuboid region, referred to as the posterior transverse arch. Another arch, the anterior transverse arch, is located at the metatarsal heads, peaking at the second, third, and fourth metatarsal heads to enhance load-bearing and elasticity of the forefoot.
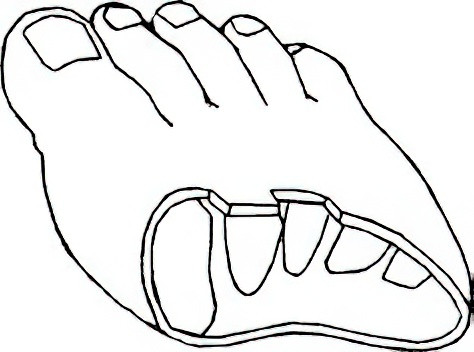
Figure 2 Transverse arch of the foot
Ligaments that maintain the arches include:
- Plantar calcaneonavicular (spring) ligament
- Long and short plantar ligaments
- Plantar aponeurosis
- Medial deltoid ligament
- Dorsal and plantar interosseous ligaments and the transverse metatarsal ligament
Leg muscles that maintain the arches include:
- Tibialis posterior, which prevents forefoot abduction and eversion and is a key stabilizer of the medial longitudinal arch and the posterior transverse arch.
- Tibialis anterior, which supports the medial longitudinal arch and prevents its collapse.
- Fibularis (peroneus) longus, which primarily maintains the posterior transverse arch.
- Flexor digitorum longus and flexor hallucis longus also contribute to the stability of the longitudinal arch.
- Gastrocnemius, contributing to the Achilles tendon at the distal one-third of the tibia and attaching to the posterior superior medial aspect of the calcaneal tuberosity, primarily limits ankle dorsiflexion and calcaneal valgus.
Etiology
The causes of flat foot are divided into congenital and acquired categories:
Congenital factors include:
- Overdevelopment of the navicular tuberosity
- Accessory navicular bone or unfused accessory epiphysis
- Calcaneal valgus
- Vertical talus
- Congenital ligament and muscle laxity
Acquired factors include:
- Prolonged weight-bearing, increased body weight, or long-distance walking leading to fatigue, which gradually weakens the soft tissues maintaining the arch—including muscles, ligaments, joint capsules, and aponeuroses—resulting in a progressive flattening of the arch.
- Prolonged bed rest due to illness, causing muscle atrophy and reduced tone, leading to arch collapse under weight-bearing.
- Poor footwear, such as high-heeled shoes, causing prolonged forward shifting of body weight and resulting in anterior and downward inclination of the calcaneus, which disrupts the longitudinal arch.
- Foot bone diseases such as rheumatoid arthritis and osteoarticular tuberculosis.
- Residual flat foot due to muscle imbalances in intrinsic and extrinsic foot muscles following poliomyelitis.
Pathology
Based on the severity of soft tissue changes, flat foot is classified into two types:
Flexible flat foot (postural flat foot) is the more common type where the soft tissues remain elastic despite being relaxed. The foot appears flat under weight-bearing but returns to normal once the weight is removed. Long-term outcomes with treatment are favorable.
Rigid flat foot (spastic flat foot) is usually caused by bone coalition (either cartilaginous or fibrous) and is difficult to correct manually.
Clinical Presentation
Early symptoms include pain on the anteromedial side of the ankle, worsening with prolonged standing or walking and improving with rest. On weight-bearing, the heel deviates into valgus, the medial side of the foot appears full, and the longitudinal arch is flattened or absent. The navicular tuberosity is prominently protruded medially, and foot impressions appear significantly enlarged. Lateral X-rays reveal a collapsed longitudinal arch and abnormal relationships among the calcaneus, navicular, cuboid, and talus. Severe cases often result in tarsal osteoarthritis.
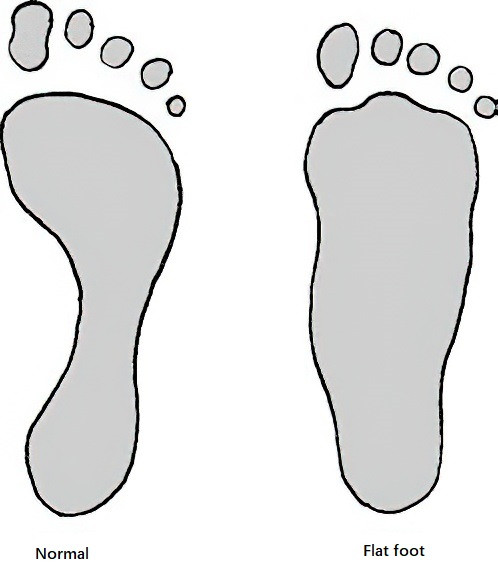
Figure 3 Normal foot and flat foot impressions
Treatment
Prevention is the primary approach. Treatment is required only if the flat foot is associated with symptoms such as pain.
For flexible flat foot, non-surgical treatment options include:
- Functional exercises, such as walking on the toes, performing toe flexion movements, and performing heel-raising with external rotation.
- Wearing orthopedic shoes or insoles. Shoes with narrow soles and arches and tightly fitting sides are recommended. The medial sole should include a 2–3 mm elevation to restore the medial longitudinal arch and support the talar head.

Figure 4 Toe flexion exercise
In rigid flat foot, rehabilitation therapy and orthopedic shoes are often ineffective. Correction under general anesthesia may involve manual inversion of the foot, followed by plaster boot fixation in the inverted and adducted position for 5–6 weeks, after which orthopedic footwear is worn. Surgical intervention is indicated for failed manual correction or severe deformities. Procedures may include:
- Subtalar arthroereisis
- Medial slipping calcaneal osteotomy
- Subtalar joint fusion
- Triple arthrodesis