Male infertility refers to the inability of a couple of reproductive age to conceive naturally within one year of regular unprotected intercourse, where the inability is attributed to factors in the male partner. According to the World Health Organization (WHO), approximately 15% of couples worldwide experience fertility problems, with male factors contributing to about 50% of cases.
Etiology
Male infertility is not a single disease but rather the result of one or more conditions or factors. Any issue affecting sperm production, maturation, ejaculation, capacitation, or fertilization may lead to infertility. The causes can be classified as follows:
- Congenital causes: These include testicular abnormalities, cryptorchidism (undescended testicles), and congenital absence of the vas deferens.
- Acquired abnormalities of the urinary and reproductive systems: Conditions such as testicular torsion, testicular trauma, testicular tumors, and orchitis can lead to testicular atrophy and result in abnormal semen parameters.
- Infections of the urinary and reproductive tract: Epididymitis, prostatitis, and seminal vesiculitis can produce excessive white blood cell by-products, such as reactive oxygen species, which damage sperm membranes. Reproductive tract infections may also cause obstruction of the vas deferens, resulting in azoospermia.
- Elevated scrotal temperature: Varicocele can raise the local temperature of the scrotum, cause local blood reflux and stasis, lead to tissue hypoxia and oxidative stress damage, and ultimately impair fertility.
- Endocrine abnormalities: Dysfunction of the hypothalamus-pituitary-testicular axis, such as in Kallmann syndrome, anterior pituitary insufficiency, hyperprolactinemia, and hyperthyroidism or hypothyroidism, is often implicated.
- Genetic abnormalities: Conditions such as Klinefelter syndrome, Y chromosome microdeletions, and primary ciliary dyskinesia can lead to infertility.
- Immune-related infertility: Surgical interventions, such as vasectomy, vasovasostomy, or testicular biopsy, may disrupt the blood-testis barrier or sperm immunosuppression mechanisms, resulting in immune infertility.
- Systemic factors: Systemic diseases, excessive alcohol consumption, drug abuse, environmental factors, and malnutrition are all contributing factors.
- Iatrogenic factors: Medical interventions, such as high doses of glucocorticoids, immunosuppressants, testicular biopsy, cryptorchidism surgery, chemotherapy, and radiotherapy, can result in semen abnormalities.
- Lifestyle factors: Obesity, smoking, and substance abuse can impact fertility. Sexual dysfunction, such as erectile dysfunction, anejaculation, or retrograde ejaculation, may also contribute.
- Idiopathic causes: About 30–50% of male infertility cases are classified as idiopathic, with no identifiable cause.
Diagnosis
Medical History
A comprehensive history should be obtained, including family history, marital and reproductive history, sexual history, fertility evaluations, treatment history, and other factors potentially affecting fertility.
Sexual History
This determines if infertility may be caused by sexual dysfunction.
Past Medical History
Specific focus should be given to reproductive history, developmental history, and medical history, including prior infections, trauma, surgeries involving the reproductive system, endocrine disorders, medications affecting testicular function or sexual health, and lifestyle factors such as alcohol consumption, smoking, and wearing tight clothing. Environmental and occupational exposures should also be considered.
Physical Examination
Systemic Examination
Particular attention should be paid to body type and secondary sexual characteristics, including patterns of body hair distribution and the presence of gynecomastia. The inguinal area should be examined for surgical scars.
Examination of the Reproductive Organs
Assessments should determine the presence of genital abnormalities, the position, consistency, and size of the testes, as well as any tenderness or masses. The epididymis and vas deferens should be evaluated for absence, thickening, nodules, or tenderness. Scrotal contents should be examined for varicocele, hydrocele, or other abnormalities.
Laboratory Testing
Semen Analysis
Semen quality assessment is a key evaluation of male fertility and should follow the standards outlined in the WHO Laboratory Manual for the Examination and Processing of Human Semen.
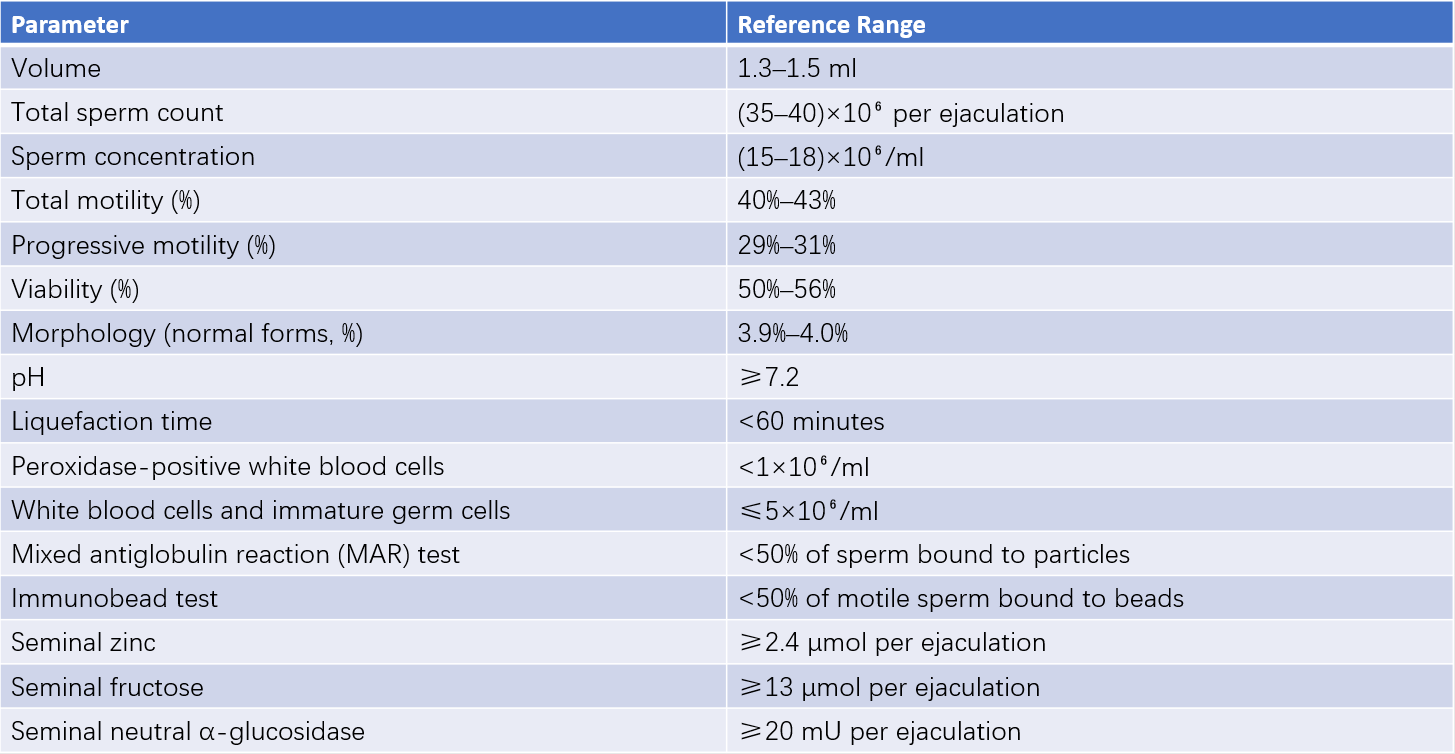
Table 1 WHO reference ranges for semen parameters (2021, sixth edition)
Selective Additional Tests
These include:
- Anti-sperm antibody testing: Recommended when postcoital tests indicate impaired sperm motility or agglutination, using methods such as the immunobead test or mixed antiglobulin reaction (MAR) test to diagnose immune-related infertility.
- Semen biochemical testing: Used to assess accessory gland function by measuring seminal fructose and neutral α-glucosidase levels, assisting in differentiating obstructive and non-obstructive azoospermia.
- Microbiological and cytological tests of the male reproductive system: Useful for identifying reproductive tract infections and evaluating the function of seminiferous tubules.
- Endocrine evaluation: Hormonal analysis is recommended as many endocrine disorders affect testicular function and fertility.
- Genetic testing: For patients with azoospermia, severe oligospermia, or a family history of infertility, karyotype analysis and Y chromosome microdeletion screening may be conducted.
- Imaging studies: Vasography or seminal vesiculography may be used to assess vas deferens patency, though these are less commonly performed. Skull imaging may exclude pituitary tumors or intracranial masses.
Specialized Testing
Testicular biopsy is performed to directly evaluate sperm production or identify the degree of spermatogenic dysfunction.
Sperm function testing is utilized to assess the functional capability of ejaculated sperm to penetrate the female reproductive tract and fertilize an egg.
Postcoital testing evaluates sperm-cervical mucus interactions.
Sexual function assessment may identify underlying sexual dysfunction contributing to infertility.
Treatment
Treatment should span at least one to two spermatogenesis cycles (3–6 months) and should involve regular evaluation of indications, efficacy, and safety. Concurrent diagnosis and treatment of both partners are important, and individualized treatment plans should be selected.
Preventive Treatment
Prevention of sexually transmitted diseases (STDs) is critical.
Early intervention for incomplete testicular descent during childhood plays a crucial role.
Safe environments should be maintained to minimize exposure to harmful factors and chemicals that can affect testicular function.
For patients undergoing treatments that may impair testicular function, such as certain medications (e.g., chemotherapy for tumors), their semen can be stored in a human sperm bank prior to treatment.
Non-Surgical Treatments
These include:
- Specific treatments: For clearly identified causes where the treatment is highly targeted, such as gonadotropin therapy for hypogonadotropic hypogonadism.
- Semi-specific treatments: For conditions where the etiology, pathology, or mechanisms are not fully clarified, such as treatment of infectious infertility or immune infertility.
- Non-specific treatments: For cases where the cause remains unknown, such as empirical or conventional medicine treatments for idiopathic oligospermia.
- General lifestyle adjustments: Improvements in lifestyle, including maintaining regular sleep patterns, controlling body weight, engaging in moderate physical activity, and limiting smoking and alcohol consumption.
- Psychological counseling and guidance on sexual activity may help reduce stress and optimize opportunities for natural conception.
Surgical Treatments
These include:
- Procedures to enhance spermatogenesis, such as high ligation of the internal spermatic vein for varicocele or orchiopexy for cryptorchidism.
- Surgery to remove obstructions in the reproductive ducts, such as vasovasostomy or epididymovasostomy.
- Surgical interventions addressing systemic diseases causing infertility, such as surgeries for pituitary tumors or thyroid disorders.
- Sperm retrieval procedures used in conjunction with assisted reproductive technologies (ART), such as microdissection testicular sperm extraction (mTESE) or microsurgical epididymal sperm aspiration (MESA).
Assisted Reproductive Technologies (ART)
ART refers to medical techniques that enable infertile couples to conceive without natural intercourse. Major ART methods include:
- Artificial insemination with husband’s semen (AIH): Processed sperm is collected and inseminated directly into the uterus (intrauterine insemination, IUI). This technique is primarily used for infertility caused by cervical factors and immune-related male infertility, with success rates around 8–10%.
- In vitro fertilization-embryo transfer (IVF-ET): Fertilization occurs in a laboratory with embryo transfer to the uterus. The success rate per cycle exceeds 30%, mainly used for treating female infertility caused by fallopian tube damage or obstruction.
- Intracytoplasmic sperm injection (ICSI): A single sperm is injected directly into the egg's cytoplasm, primarily for severe oligospermia, necrospermia, or obstructive azoospermia. The fertilization success rate can reach approximately 70%, with pregnancy rates of 35–50% when two embryos are transferred.
- Artificial insemination with donor’s semen (AID): This method is considered for male infertility unresponsive to other treatments when the female partner has normal fertility, with the goal of assisting reproduction.