Primary hyperaldosteronism (PHA), also known as Conn's syndrome, is a condition caused by excessive secretion of aldosterone from the zona glomerulosa of the adrenal cortex. The major symptoms include hypertension, hypokalemia, hypernatremia, low plasma renin levels, metabolic alkalosis, muscle weakness, or periodic paralysis. The disease was first described by Conn in 1953. Among hypertensive patients, the prevalence of PHA is estimated to be between 0.5% and 20%, making it the most common cause of secondary hypertension.
Etiology and Pathology
Idiopathic Hyperaldosteronism (IHA)
IHA is the most common subtype of PHA, accounting for approximately 60% of cases. Patients with IHA often present with atypical symptoms. Its pathological features include bilateral adrenal zona glomerulosa hyperplasia. IHA is associated with aldosterone-stimulating factors produced by the pituitary gland and is sensitive to angiotensin. Although renin activity is suppressed, the condition still responds to stimuli such as postural changes. Aldosterone secretion and clinical manifestations in IHA are generally milder compared to adenoma-type cases.
Aldosterone-Producing Adrenal Adenoma (APA)
APA, also known as aldosteronoma, accounts for approximately 35% of PHA cases. These tumors are typically solitary and unilateral, with aldosterone production independent of renin or angiotensin II. About 90% of APAs are unilateral, more commonly on the left side, while bilateral APAs are rare, comprising approximately 10% of cases. These tumors are usually round, golden-yellow in color, and have a diameter of 1–2 cm.
Unilateral Adrenal Hyperplasia (UNAH)
UNAH is relatively rare and is characterized by nodular hyperplasia of the zona glomerulosa in one adrenal gland. Its endocrine and biochemical features are similar to APA and result in the typical symptoms of PHA.
Aldosterone-Producing Adrenocortical Carcinoma (ACC)
ACC is an uncommon cause of PHA. These tumors typically measure more than 5 cm in diameter, present irregular shapes, and exhibit uneven densities with necrosis and calcification. The disease progresses rapidly, and surgical, pharmacological, or radiation treatments are often of limited effectiveness.
Ectopic Aldosterone-Producing Tumors
These tumors are extremely rare and may arise from adrenal remnants located in the kidney or ovarian tumors. Cells in ectopic tumors are capable of aldosterone secretion but do not respond to ACTH or angiotensin.
Familial Hyperaldosteronism (FH)
FH is divided into four subtypes:
- FH-I (glucocorticoid-remediable aldosteronism, GRA): This is an autosomal dominant condition characterized by relatively mild hypertension and hypokalemia, which are unresponsive to conventional antihypertensive drugs. Glucocorticoids, however, can help maintain normal blood pressure and potassium levels.
- FH-II: This is also an autosomal dominant disease that can be cured or significantly improved through adrenalectomy.
- FH-III: This type is associated with mutations in the KCNJ5 gene, leading to increased aldosterone secretion by adrenal cells.
- FH-IV: This form is more commonly seen in children under the age of 10 and is associated with cognitive impairment, seizures, and autism symptoms in addition to PHA. Diagnosis can be confirmed through CACNA1H gene testing.
Clinical Manifestations
Hypertension
PHA is usually characterized by moderate to severe resistant hypertension, primarily with elevated diastolic blood pressure. The condition responds poorly to antihypertensive medications.
Hypokalemia
Approximately 70% of patients exhibit persistent hypokalemia, while 30% have intermittent hypokalemia. Symptoms of hypokalemia include muscle weakness and, in severe cases, periodic paralysis. Paralysis commonly starts in the limbs and may lead to flaccid paralysis, affecting breathing or swallowing in critical situations. Hypokalemia also causes electrocardiographic changes and impaired physiological reflexes.
Polydipsia, Polyuria, and Nocturia
These symptoms are primarily caused by hypokalemia, which leads to vacuolar degeneration of renal tubular epithelial cells and reduced renal concentration ability. Increased aldosterone secretion causes sodium retention. The resulting hypernatremia triggers polydipsia.
Elevated Fasting Blood Glucose
Chronic hypokalemia affects insulin secretion, leading to elevated fasting blood glucose levels in approximately 25% of PHA cases.
Auxiliary Examinations
General Laboratory Tests
Findings typically include hypokalemia, hypernatremia, metabolic alkalosis, normal-to-elevated blood CO2 binding capacity, and elevated urinary pH. Increased urinary potassium excretion, elevated plasma and urinary aldosterone levels, and reduced plasma renin activity are also observed.
Specialized Tests
Spironolactone Test
Spironolactone, a synthetic competitive aldosterone antagonist, may be administered for 2–3 weeks. This tends to result in reduced blood pressure, increased serum potassium, reduced urinary potassium excretion, improvement in muscle weakness, decreased serum sodium, increased urinary sodium excretion, normalized CO2 binding capacity, and acidification of the urine.
Plasma Aldosterone Concentration (PAC)/Plasma Renin Activity (PRA) Ratio (ARR)
The ARR is used as a screening test for PHA. The diagnosis of PHA is supported when PAC >15 ng/dl, PRA >0.2 ng/(ml·h), and the PAC-to-PRA ratio exceeds 30:1.
Postural Test
Aldosterone concentration and renin activity are measured in the morning while lying down and again after 4 hours of upright activity. In normal individuals and non-PHA patients, standing increases renin activity and angiotensin levels slightly, while aldosterone concentrations may increase 2–4 times. In idiopathic hyperaldosteronism (IHA), aldosterone levels increase by at least 33%, whereas no significant change is observed in cases of adenoma.
Other Confirmatory Tests
Tests include high-sodium diet loading, fludrocortisone suppression, saline infusion, and captopril suppression.
Dexamethasone Suppression Test
This test is used to identify glucocorticoid-remediable aldosteronism (GRA). Following the administration of dexamethasone (2 mg once daily for three weeks), normalization of serum potassium, blood pressure, and aldosterone secretion indicates the diagnosis.
Adrenal Venous Sampling (AVS)
AVS is primarily used in patients with bilateral adrenal lesions to determine the dominant side of hormone secretion. It involves measuring aldosterone and cortisol concentrations in adrenal veins and the inferior vena cava. A unilateral aldosterone-to-cortisol ratio greater than 4 in the adrenal vein indicates the dominant side and is critical for preoperative functional localization.
Localization Studies
Ultrasound (US)
This is commonly used in the screening of adrenal tumors, particularly for masses >1 cm in diameter. However, it has a low detection rate for lesions smaller than 1 cm.
CT Scanning
Adrenal adenomas typically appear as hypodense or isodense masses with minimal enhancement. CT has a detection rate exceeding 90% for APA lesions smaller than 1 cm. Thin-slice CT is valuable for detecting adrenal nodules or hyperplasia less than 1 cm in diameter. UNAH generally presents as unilateral adrenal enlargement or nodular changes, while IHA presents as bilateral adrenal enlargement.
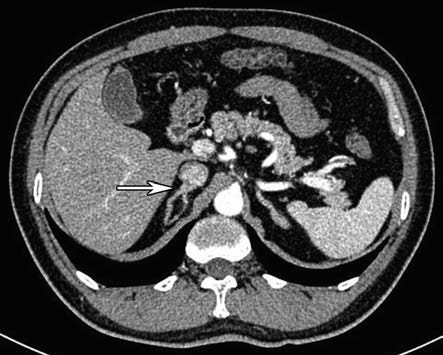
Figure 1 CT image of right adrenal aldosterone tumor
MRI Scanning
MRI offers higher specificity and is especially useful for comparing in-phase and out-of-phase images. MRI is also suitable for pregnant patients and those who cannot tolerate intravenous contrast agents.
68Ga-pentixafor-PET-CT
This imaging modality may play an important role in the subtype diagnosis of PHA.
Treatment
Surgical Management
Surgical removal is the first-line treatment for APA, involving resection of the tumor and the ipsilateral adrenal gland, which often cures the condition. Unilateral adrenalectomy or subtotal adrenalectomy is effective for UNAH. Radical tumor resection is recommended for aldosterone-producing adrenocortical carcinomas (ACC) and ectopic aldosterone-producing tumors. IHA responds poorly to adrenal surgery and is primarily managed with medications. Laparoscopic adrenalectomy is the preferred surgical approach for APA, UNAH, and related conditions.
Preoperative preparation aims to control hypertension, correct hypokalemia, and address metabolic alkalosis. Common medications used for preoperative preparation include:
- Spironolactone: The first-line medication. High doses of spironolactone, combined with potassium supplements and long-acting antihypertensive drugs, normalize blood pressure and potassium levels in most patients within 5–7 days, optimizing them for surgery.
- Amiloride: A long-acting potassium-sparing diuretic.
- Triamterene: A diuretic that works on the distal renal tubules to inhibit sodium reabsorption.
- Other Medications: These include ACE inhibitors (e.g., captopril or ramipril) and calcium channel blockers (e.g., nifedipine), often used in combination with potassium-sparing diuretics or spironolactone. They rapidly restore potassium and blood pressure to normal levels. Adequate potassium supplementation and a low-sodium, high-potassium diet may also be required preoperatively.
Medical Therapy
Medication is the mainstay of treatment for IHA and GRA. If patients cannot tolerate medication due to side effects, surgery may be considered to remove the dominant or larger adrenal gland responsible for aldosterone secretion.