The membranous urethra traverses the urogenital diaphragm. During pelvic fractures, the sudden displacement of the urogenital diaphragm attached to the inferior pubic ramus generates shearing forces, leading to laceration of the membranous urethra or even complete transection at the prostatic apex. Tearing of the puboprostatic ligament causes upward and posterior displacement of the prostate. Fractures and injury to the pelvic vascular plexus may result in significant hemorrhage, forming large hematomas around the prostate and bladder. Following posterior urethral disruption, urine can extravasate from the prostatic apex into the retropubic space and perivesical regions.
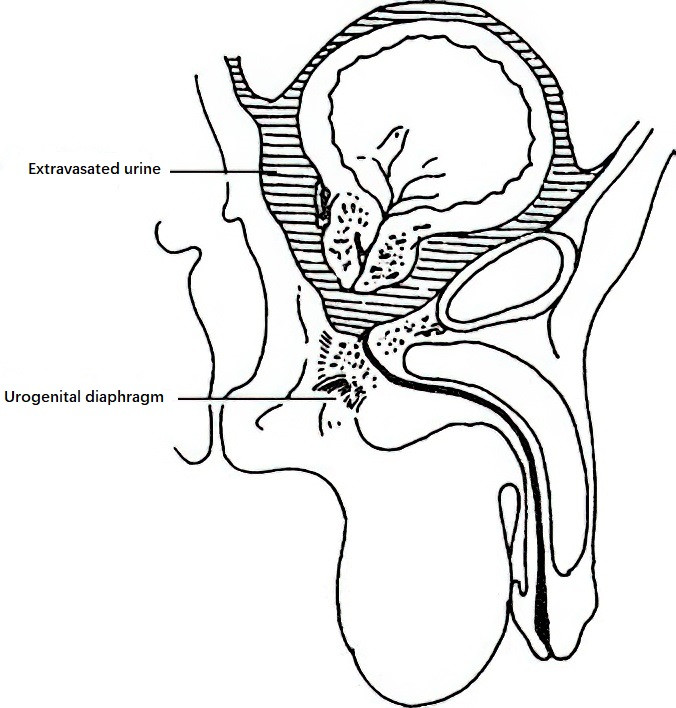
Figure 1 The range of urine extravasation in posterior urethral injury
Clinical Manifestations
Shock
Posterior urethral injuries resulting from pelvic fractures are often severe and commonly involve significant bleeding, leading to traumatic or hemorrhagic shock.
Pain
Symptoms include lower abdominal pain, local muscle tension, and tenderness. As the condition progresses, abdominal distension and reduced bowel sounds may develop.
Difficulty in Urination
Disruption or blockage of urethral continuity caused by laceration or rupture of the urethra often leads to difficulty in urination and urinary retention.
Urethral Bleeding
Minimal or no blood is observed at the external urethral meatus.
Urine Extravasation and Hematoma
Urine extravasation in posterior urethral injuries typically occurs in the retropubic space and around the bladder. In cases of urogenital diaphragm rupture, hematomas and urine extravasation appear in the perineum and scrotum.
Diagnosis
Medical History and Physical Examination
Posterior urethral injury should be considered in cases of pelvic crush injuries accompanied by urinary retention. Rectal examination may reveal a soft hematoma in the anterior rectal wall with tenderness, and the prostate apex may feel mobile. Bloodstains on the examiner’s glove suggest associated rectal injury.
X-ray and Contrast Studies
Anteroposterior pelvic radiographs reveal pelvic fractures. Retrograde urethrography combined with cystography through a suprapubic cystostomy assists in determining the location and severity of posterior urethral injury.
Treatment
Emergency Management
Patients with pelvic fractures are recommended to remain in a supine position without unnecessary movement. Severe trauma with significant bleeding may result in shock, necessitating anti-shock therapy.
Early Management
Foley Catheterization
Catheterization may be attempted in cases of mild injuries involving partial posterior urethral rupture. Successful catheterization warrants the retention of the catheter for two weeks. Catheterization should not be performed in cases of severe injury to avoid exacerbating local damage or causing hematoma infection.
Suprapubic Cystostomy
Patients with urinary retention may undergo high suprapubic cystostomy under local anesthesia. The cystostomy tube should only be removed after confirming the absence of urethral strictures or urine extravasation via bladder urethrography. Persistent urinary retention necessitates scar excision and end-to-end urethral anastomosis three months after cystostomy.
Urethral Realignment Surgery
Early restoration of urethral continuity may be achieved in some patients using a urethral realignment procedure to prevent scar channel formation due to retraction of the severed urethral ends. The surgical method involves a midline lower abdominal incision to evacuate the retropubic hematoma and open the bladder. The surgeon's index finger is inserted through the bladder neck into the posterior urethra to guide a urethral sound introduced through the external urethral meatus into the bladder. A regular Foley catheter attached to the sound's tip is pulled through the urethra to the bladder. A cystostomy tube is also secured to the catheter tip and brought out through the cystostomy exit to prevent catheter displacement due to balloon rupture. Traction is applied to the balloon catheter toward the external urethral meatus to realign the severed urethral ends. The catheter is secured with adhesive tape to the inner thigh for skin traction. Traction is released after approximately two weeks, and the catheter is left in place for another one to two weeks. Smooth urination following this treatment may preclude the need for a second-stage urethral anastomosis.
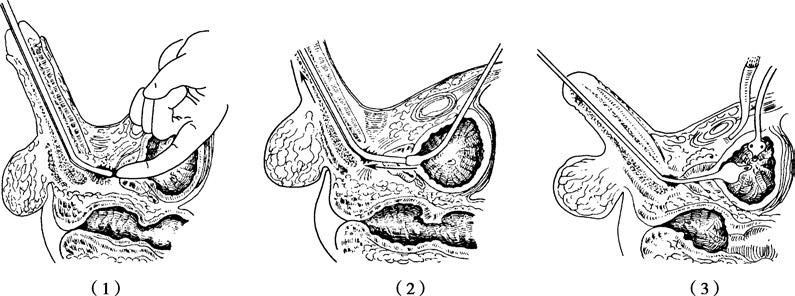
Figure 2 Urethral realignment surgery
Management of Complications
Urethral Stricture
Urethral stricture is a common complication of posterior urethral injury. Weekly urethral dilation is recommended after removal of the catheter for one month, followed by regular dilation thereafter. For patients with cystostomies, stricture or obstruction occurring three months later may require second-stage surgical intervention, such as transurethral incision or excision of constricted scar tissue, or excision through a perineal approach followed by end-to-end urethral anastomosis.
Rectal Injuries
Posterior urethral injuries combined with rectal injuries necessitate early repair procedures, with the potential need for temporary colostomy.
Urethrorectal Fistula
Repairs for urethrorectal fistulas are deferred for three to six months following their development.