Bile duct cancer refers to malignant tumors that occur in the extrahepatic bile ducts, from the left and right hepatic ducts to the lower end of the common bile duct. With advances in diagnostic techniques, the detection rate of this disease has significantly increased.
Etiology
The exact cause remains unclear. This cancer predominantly occurs in individuals aged 50 to 70, with a male-to-female ratio of approximately 1.4:1. Several factors may be associated with its development, including:
- Hepatobiliary stones, as approximately one-third of bile duct cancer cases are associated with biliary stones, and 5%–10% of patients with biliary stones may develop bile duct cancer.
- Primary sclerosing cholangitis.
- Congenital bile duct dilation or biliary cysts, especially after choledochojejunostomy.
- Ulcerative colitis.
Location
Based on the location of the tumor, bile duct cancer is classified into upper, middle, and lower segments:
Upper Segment Cancer (Hilar Cholangiocarcinoma)
Also known as hilar bile duct cancer, it occurs in the region between the left and right hepatic ducts and above the opening of the cystic duct, representing 50%–75% of cases. The classification proposed by Bismuth-Corlette divides hilar cholangiocarcinomas into four subtypes:
- Type I: Tumor located in the common hepatic duct, without involvement of the confluence of the left and right hepatic ducts.
- Type II: Tumor involves the confluence of the hepatic ducts but not the left or right hepatic ducts.
- Type IIIa: Tumor invades the right hepatic duct.
- Type IIIb: Tumor invades the left hepatic duct.
- Type IV: Tumor involves both the left and right hepatic ducts.
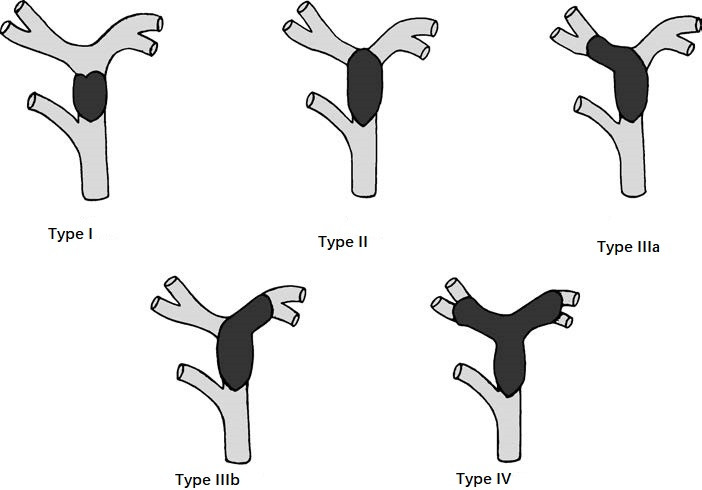
Figure 1 Bismuth-Corlette classification for hilar cholangiocarcinoma
Middle Segment Cancer
This is located between the opening of the cystic duct and the superior margin of the duodenum, accounting for 10%–25% of cases.
Lower Segment Cancer
This is found between the superior margin of the duodenum and the ampulla of Vater, comprising 10%–20% of cases.
Pathology
Macroscopic Types
Papillary type is most commonly seen in the lower bile duct. These appear as polyp-like projections into the lumen, sometimes associated with abundant mucus secretion.
Nodular type is small, localized tumors presenting as thickened bile duct walls with nodules projecting into the lumen, more commonly in the middle bile duct.
Sclerosing type exhibits extensive thickening of the bile duct wall and luminal narrowing, often accompanied by periductal fibrosis, making it difficult to distinguish from sclerosing cholangitis.
Histological Types
Adenocarcinoma accounts for over 95% of cases, predominantly well-differentiated, with a smaller proportion being poorly differentiated or undifferentiated. The tumor typically grows slowly, and the primary modes of spread include lymphatic metastasis, local invasion, and peritoneal seeding. The tumor infiltrates longitudinally along the bile duct wall, both proximally and distally, as well as circumferentially into nearby structures, such as the liver, blood vessels, and nerve sheaths. Lymphatic metastasis occurs along the hepatic artery to lymph nodes around the common hepatic artery, celiac artery, pancreatic margin, posterior duodenum, and retroperitoneal regions. Other rare types include squamous carcinoma, adenosquamous carcinoma, and carcinoid.
Clinical Manifestations and Diagnosis
Jaundice
Painless jaundice is the primary clinical feature, which progressively worsens. Stool may appear pale or clay-colored, and pruritus may be present. Symptoms such as loss of appetite, fatigue, anemia, and weight loss are also common.
Gallbladder Enlargement
Tumors in the middle or lower bile duct may cause an enlarged, palpable gallbladder. In cases of hilar cholangiocarcinoma, the gallbladder may not enlarge and could even appear contracted.
Hepatomegaly
Persistent jaundice can lead to liver damage, resulting in hepatomegaly, ascites, or lower extremity edema. Tumor invasion of the portal vein may lead to portal hypertension and, potentially, upper gastrointestinal bleeding.
Fever and Upper Abdominal Pain
Secondary biliary infection can result in fever and abdominal pain.
Laboratory Tests
Elevated serum total and direct bilirubin levels and progressively increased alkaline phosphatase (ALP), gamma-glutamyltransferase (GGT), ALT, and AST levels can be observed. Biliary obstruction can impair vitamin K absorption, reducing the liver's ability to synthesize coagulation factors and prolonging prothrombin time. Elevated tumor markers such as CA19-9 and CEA can aid in diagnosis.
Imaging Studies
Ultrasound shows intrahepatic bile duct dilation and thickening of the extrahepatic bile duct wall or intraductal masses. High-frequency endoscopic ultrasound reduces interference from intestinal gases and can assess tumor infiltration depth; direct biopsy can also be performed through this method.
CT and MRI biliary imaging helps in identifying the site of biliary obstruction and the nature of the lesion.
Percutaneous transhepatic cholangiography (PTC) provides clear imaging of the bile duct and its lesions.
Endoscopic retrograde cholangiopancreatography (ERCP) is useful for diagnosing and managing lower bile duct cancer.
Treatment
Radical Surgical Resection
Radical surgical resection is the preferred and most effective treatment for this disease. The surgical approach differs depending on the location of the bile duct cancer.
Upper Segment Bile Duct Cancer (Hilar Cholangiocarcinoma)
For Bismuth-Corlette type I and some type II hilar cholangiocarcinomas, removal of the gallbladder and extrahepatic bile ducts is sufficient, followed by biliary reconstruction with Roux-en-Y hepaticojejunostomy. For some type II, IIIa, or IIIb cases, in addition to gallbladder and extrahepatic bile duct removal, limited liver resection may be necessary (e.g., resection of segment IV or segments IV+V). For a small number of patients, ipsilateral hemihepatectomy with or without resection of the caudate lobe may be required. The extent of resection varies with the cancer type, but lymph node dissection from the hepatoduodenal ligament is essential, achieving thorough "vascular skeletonization" of the hepatoduodenal ligament. Depending on the number and diameter of the bile ducts at the residual liver margin, biliary reconstruction can involve either standard bile-intestinal anastomosis or an anterior wall hepaticojejunostomy (Chen’s hepaticointestinal anastomosis). For most type IV hilar cholangiocarcinomas, resection is not feasible, and chemotherapy, targeted therapy, and/or immunotherapy may be initiated. If effective, the possibility of surgical resection can be reconsidered.
Middle Segment Bile Duct Cancer
Resection involves removing the tumor along with approximately 1.0 cm of bile duct margins on either side, achieving "vascular skeletonization" of the hepatoduodenal ligament, followed by Roux-en-Y hepaticojejunostomy for biliary reconstruction.
Lower Segment Bile Duct Cancer
Surgical treatment involves pancreaticoduodenectomy. For tumors that invade the liver, pancreas, or duodenum, combined hepato-pancreaticoduodenectomy may be performed. In rare cases, complete cure can be achieved.
Palliative Therapy
Palliative treatments are used for unresectable bile duct cancers.
Biliary Drainage
Percutaneous transhepatic cholangial drainage (PTCD) or placement of an internal stent.
Endoscopic nasobiliary drainage (ENBD) or placement of an internal stent to relieve jaundice. If the tumor is found to be unresectable during surgery, internal biliary drainage through hepatic-enteric or bile duct-enteric anastomosis may be performed.
Gastrojejunostomy
For cases where the tumor invades or compresses the duodenum causing gastrointestinal obstruction, gastrojejunostomy can be performed to restore digestive continuity and improve the patient’s quality of life.
Pharmacological Therapy
For advanced cases, chemotherapy regimens based on gemcitabine are commonly used, often in combination with platinum-based drugs and immunotherapy. If genetic testing identifies specific molecular targets, immunotherapy combined with targeted therapy has demonstrated favorable results.