Etiology and Pathology
Acute acalculous cholecystitis accounts for approximately 5% of acute cholecystitis cases. The exact cause is unclear, but it typically occurs in critically ill patients, such as those with severe trauma, burns, or abdominal non-biliary surgeries, including abdominal aortic aneurysm repair, as well as those with sepsis. Around 70% of affected individuals have accompanying atherosclerosis. Some researchers also associate this condition with prolonged parenteral nutrition or as a complication of immunodeficiency diseases such as AIDS. Pathological changes are similar to those of acute calculous cholecystitis, but the progression is more rapid. The primary pathogenic factors include bile stasis and ischemia of the gallbladder wall, leading to rapid bacterial proliferation and reduced blood supply, with an increased likelihood of gallbladder gangrene and perforation.
Clinical Manifestations
This condition is more common in older male patients. Its clinical presentation is similar to that of acute calculous cholecystitis. However, symptoms of abdominal pain are often masked by the presence of other severe underlying conditions, increasing the risk of misdiagnosis and delayed treatment.
For critically ill patients, such as those with severe trauma or on prolonged parenteral nutrition, the occurrence of right upper abdominal pain accompanied by fever should raise concern for this condition. Signs such as right upper abdominal tenderness, positive peritoneal irritation signs, palpable enlarged gallbladder, or positive Murphy's sign should prompt further investigation. Early detection via ultrasound can be challenging, but CT imaging may provide diagnostic insights, and hepatobiliary scintigraphy offers diagnostic confirmation in about 97% of cases.
Treatment
This condition is prone to complications such as gangrene and perforation. Once diagnosed, prompt surgical intervention is warranted. Treatment options include cholecystectomy, cholecystostomy, or percutaneous transhepatic gallbladder drainage (PTGD). For patients without a confirmed diagnosis or with less severe symptoms, aggressive non-surgical management under close observation can be pursued. Surgical intervention should be implemented promptly if the condition worsens.
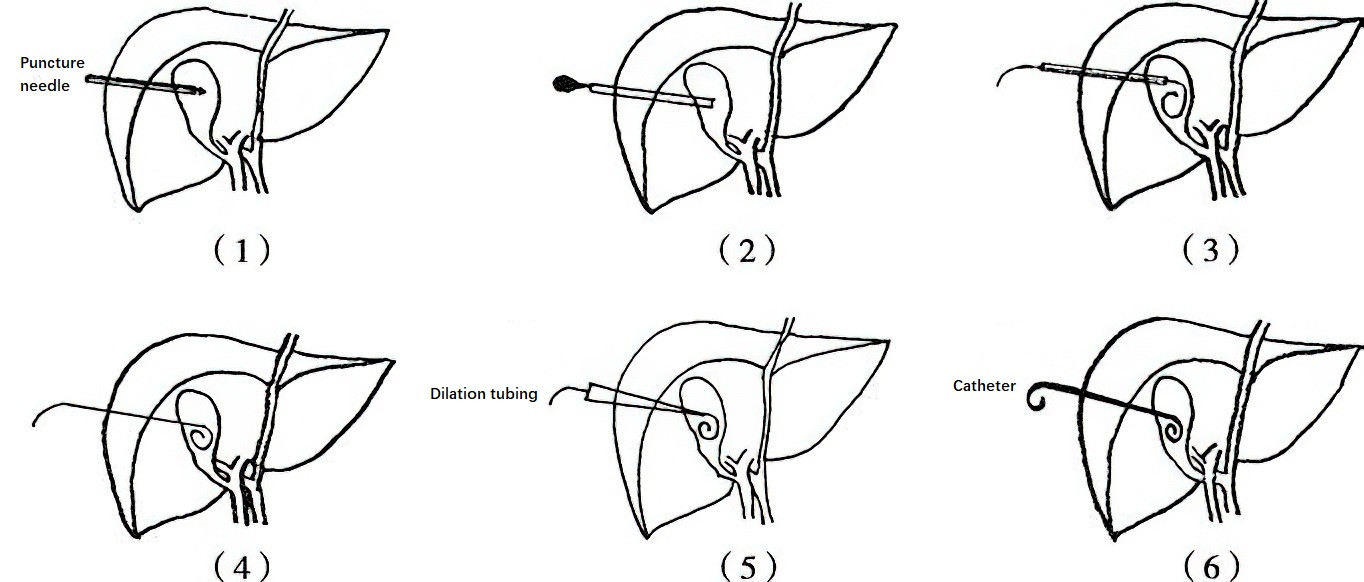
Figure 1 Percutaneous transhepatic gallbladder drainage procedure
1, Insertion of the puncture needle into the gallbladder.
2, Removal of the needle's inner core.
3, Placement of a guidewire.
4, Withdrawal of the cannula.
5, Expansion of the skin puncture site with dilation tubing.
6, Placement of the drainage catheter over the guidewire, followed by removal of the guidewire and securing of the catheter to the skin near the puncture site.