Budd-Chiari syndrome refers to a group of diseases characterized by portal hypertension or both portal and inferior vena cava hypertension due to congenital or acquired obstruction of the hepatic veins and/or the inferior vena cava above their openings. The condition can lead to congestive hepatic fibrosis and cirrhosis.
Etiology
In Western countries, the syndrome is primarily caused by hepatic vein thrombosis resulting from a hypercoagulable state, such as myeloproliferative diseases or antithrombin III deficiency. In Asian countries, inferior vena cava obstruction is more common, potentially related to congenital developmental abnormalities, thrombus organization, local trauma, or environmental factors.
Classification
Although there is no standardized classification system, the syndrome is typically divided into three types based on the location of the lesions:
- Inferior vena cava type: Characterized by stenosis or obstruction primarily caused by membranes in the inferior vena cava.
- Hepatic vein type: Characterized by obstruction of the major hepatic veins.
- Mixed type: Involves simultaneous obstruction of the hepatic veins and inferior vena cava.
Clinical Presentation
The clinical manifestations vary depending on the number and extent of vascular involvement, as well as the nature and condition of the obstructive lesions. Acute, subacute, and chronic presentations can occur. Symptoms typically reflect portal hypertension, such as ascites, esophagogastric varices with associated gastrointestinal bleeding, and splenomegaly. Symptoms of inferior vena cava hypertension may also be present, including hepatosplenomegaly, varices of the thoracoabdominal and lower limb veins, and skin pigmentation. Chronic cases may involve severe ascites, malnutrition, and a characteristic "spider-like" body habitus.
Diagnosis
Ultrasound, CTA, and MRA serve as the primary diagnostic modalities.
Direct signs include detection of stenosis or obstruction in the hepatic veins or inferior vena cava, as well as identification of collateral venous pathways.
Indirect signs include caudate lobe enlargement and the formation of sclerotic nodules.
Treatment
Interventional Therapy
Interventional treatment is the first-line approach and primarily involves balloon angioplasty of the inferior vena cava or hepatic veins, with stent placement when necessary. Transjugular intrahepatic portosystemic shunt (TIPS) procedures are effective in reducing portal venous pressure.
Surgical Therapy
Surgical treatment remains an important option but has declined in clinical usage.
For inferior vena cava obstruction, diaphragmatic membrane excision and thrombectomy or inferior vena cava–right atrium bypass procedures may be performed.
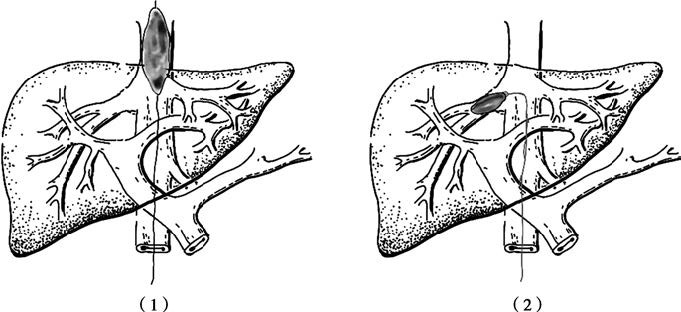
Figure 1 Balloon angioplasty
(1) Inferior vena cava balloon angioplasty
(2) Hepatic vein balloon angioplasty
For hepatic vein obstruction, portosystemic shunt surgeries such as mesocaval shunt, portocaval shunt, or splenorenal shunt may be options. Procedures like modified splenopulmonary fixation have also been considered.
Liver transplantation is recommended for patients in the terminal stage of disease.
Prognosis
The long-term prognosis for this condition remains poor. Postoperative recurrence is common, and patients often succumb due to liver failure or gastrointestinal bleeding. Survival time is closely associated with the type of lesions and the degree of liver function impairment. Early diagnosis and treatment can improve survival rates.